Salzmann’s Nodular Degeneration
By Martin Conway & Mark Darling
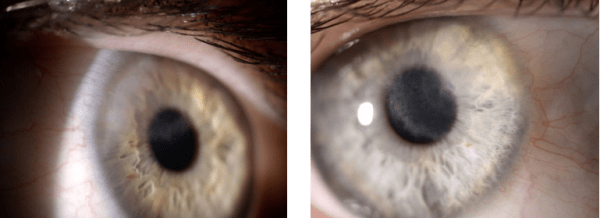
RE + LE
Salzmann’s Nodular Degeneration (SND) is a non-inflammatory, progressive corneal degeneration, characterised by elevated, whitish-grey subepithelial nodules. The nodules are developed by fibrous overgrowth and may appear at any part of the cornea. Patients can present with unilateral or bilateral disease and the number of nodules can vary from one to many. It is most commonly seen in females and is more usual although not limited to elderly patients in their 7th, 8th or 9th decade.
SND has been associated with several ocular pathologies including meibomian gland dysfunction, chronic blepharitis, trichiasis, trachoma, previous ocular trauma, Thygeson’s punctate keratitis, vernal keratitis, filamentary keratitis, chronic uveitis, phlyctenular keratitis, and epithelial basement membrane dystrophy. Previous ocular trauma and previous surgery including cataract extraction, pterygium excision, and laser-assisted in situ keratomileusis (LASIK), and long-term use of contact lenses, especially soft lenses, have also been associated with SND. The common factor among all of the conditions associated with SND is poor epithelial protection, due to chronic irritation or mechanical disruption of the epithelial-stromal barrier during trauma or surgery, which is thought to be important in the development of SND. However, it is important to remember that conditions such as meibomian gland dysfunction and contact lens use are prevalent in the population and their co-existence with SND does not necessarily imply causation.
Development of SND after LASIK has been reported multiple times. Given the presentations of SND both proximal and remote from the LASIK history, the trigger for post-LASIK SND may be surgical trauma, anatomical disruption in the area of the flap, and/or post-operative dry eye disease.
Symptoms
Patients usually present with a gradual loss of vision at both distance and near due to significant irregular astigmatism caused by the nodules. Patients may also present with a foreign body sensation on the surface of the cornea. Slit lamp examination can reveal white to bluish-grey nodules within the cornea.
Whilst decreased visual acuity, epiphora, photophobia and chronic foreign body sensation are common symptoms, SND may be asymptomatic in 15% of cases.
Management
There is no report of spontaneous resolution. Treatment to date involved surgical or medical intervention dependent upon the severity of the symptoms.
Medical treatments include ocular lubricants, steroid eye drops, warm compresses and attention to lid care as per dry eye. Surgical indications would be ocular discomfort or reduced acuity due to irregular astigmatism.
Scleral Lenses
The following case indicates that scleral lenses may offer an alternative to surgery when medical treatments fail to achieve satisfactory comfort and/or visual acuity comfort.
Case Study – Salzmann’s Nodular Degeneration R&L
Patient SP, Female, age 31
History
Diagnosed SND 10 years, managed with lubricants until recently when visual acuity and comfort deteriorated. Struggling with night driving and distortion due to astigmatism.
Vision
R 6/19. Spec Rx +2.00/-3.00 x20 = 6/9.5
L 6/9.5. Spec Rx +1.00/-1.50×160 = 6/6
Topography at initial visit:
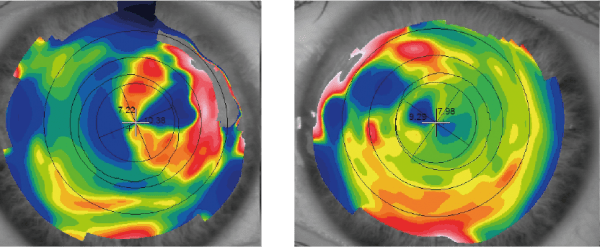
Original Topography R and L
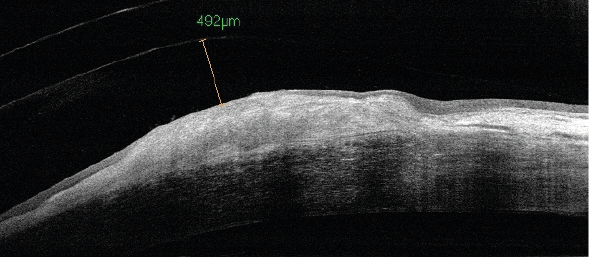
OCT RE at initial visit, disrupted surface, 492μm clearance
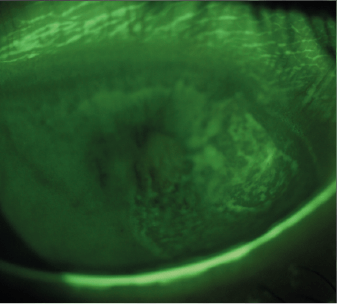
RE S/Lamp + FL
Lenses
Because of the position and height of the nodule in the RE in particular, it was decided to fit with a much higher clearance centrally than normal in order to allow for future growth in size of the nodule. Clearance at fitting was 492 microns over the nodule. It was decided to observe progress and adjust if necessary.
At 6/12 follow up, Px reported some issues in air-conditioned environments, some issues with mild hay fever, but significantly improved comfort. Slight conjunctival prolapse noted due to excessive central clearance and mild superficial punctate keratitis. HycoSan Extra issued for use in bowl upon insertion. Visual acuities 6/6 R&L.
At 12/12 follow up. Wearing time 15 hours in comfort, occasional clouding but patient is happy to remove the lenses and refresh the bowl solution. Vision is now 6/6 in both eyes and night driving is much better with less distortion. Patient feels spec Rx may have changed.
OCT shows that R nodule is less pronounced, clearance over the nodule has increased to 585 microns, meaning that the nodule has shrunk by nearly 100 microns. Spec refraction now shows a change in axis of astigmatism with improvement in acuity due to reduction in corneal irregularity.
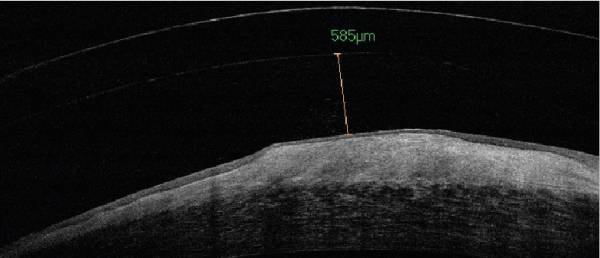
OCT @ 1 year check, 585μm clearance
Consider reducing sag on future lenses, possibly using reverse curve to reduce central clearance. Leave for time being as patient progressing well.
Summary
Even though the sag was excessive, comfort – which was the main problem – is no longer an issue.
The nodule appears to have benefitted from being constantly bathed in saline/HycoSan, and the subsequent reduction in its size has reduced the irregular astigmatism and improved vision.
The use of sclerals, made in Optimum Extreme material, in this case, has negated the need for a surgical procedure which would have been the only other option.

Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. He is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). Martin has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
More articles by Martin Conway:

Mark Darling is a graduate of City University, London. He completed his pre-registration year in the Contact Lens Department of Moorfields Hospital in London, and has had his own practice since 1990. Mark has a special interest in speciality lens fitting and assists in clinical trials for Contamac. He also works closely with a local hospital eye department and has built a substantial scleral patient base using designs from many of Contamac’s laboratory partners.
