The Evolution of Scleral Lens Fitting
By Martin Conway
Scleral lens fitting has become increasingly mainstream over the past decade. Once the preserve of specialist practice and confined mainly to hospital practice, it has become the fastest-growing lens choice for irregular corneal problems from keratoconus, ectasia and increasingly for dry eye disorders.
“Traditional” scleral lenses consist of three zones, a central optical zone which vaults the cornea and extends to around 10mm, a landing zone which bears the weight of the lens and aligns with the sclera which extend from around 12.5 mm to the edge of the lens, and an intermediate or limbal zone which links the other two and extends over the limbus – hence the name. These zones originally consisted of three gradually flattening curves in a similar manner to a conventional C3 corneal lens. This brought the limbal zone into close contact with the limbus, particularly in the upper nasal quadrant as the lens displaced downwards and temporally with wear.
As lenses became more widely fitted, particularly in the United States, practitioners and researchers began to voice concern about this region of the cornea and risks to the production of limbal stem cells. Opinion leaders suggested that lenses should be fitted with greater limbal clearance and lens designers began to include reverse curves into the limbal zone in order to lift this part of the lens away from this important area and prevent any insult or pressure in this region.
Raising the profile of the lens in this way increased the volume of the post lens tear layer and we then began to see the phenomenon of “fogging” reported in around 30% of cases.
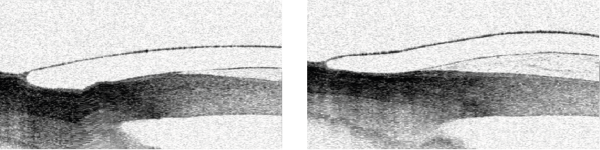
Figure 1: Traditional Design with close alignment over limbus and Figure 2: Same Eye with reverse curve to increase limbal clearance
It is now generally thought that this phenomenon is due to extraneous lipid, mucous and cellular debris being sucked under the lens edge during the blink when the lens edge is not aligned with the scleral shape. The conjunctiva can also be sucked under a loose lens edge by this pump mechanism causing what is known as a conjunctival prolapse.
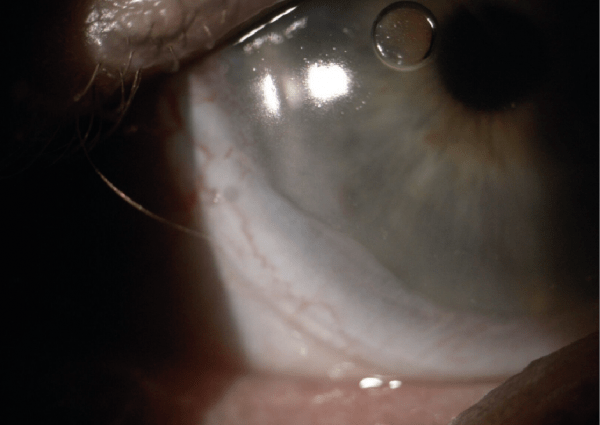
Figure 3: Conjunctival Prolapse
As we became more knowledgeable about the scleral shape, it became more usual for manufacturers to offer their lenses with a toric periphery in order to prevent this backwash under the lens. It soon became obvious that, unlike all previous lens types, we are actually fitting the lens to the scleral rather than the cornea. Corneal shape was less indicative of success than how the lens was aligned over the sclera. Whilst is desirable to closely align to back surface of the lens with the corneal shape, patients could tolerate lenses fitted at 500 microns and more clearance, as long as the edge was functioning properly.
The use of OCT technology proved to provide practitioners with a much more accurate method of assessing lens clearances than fluorescent alone, but could not provide any accurate indication of lens shape prior to fitting.
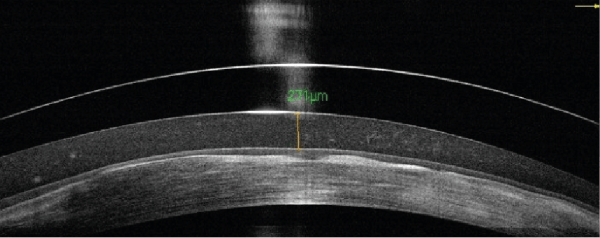
Figure 4: OCT image showing clearance and fogging
Combining 3D scanning algorithms with a traditional method of obtaining an impression mould allowed for the production of extremely accurate scleral peripheries capable of allowing for almost all irregularities in shape including pingueculae and even stents. This method, whilst effective is time-consuming, expensive and a little daunting for all but the hardiest patients.

Figure 5: Scleral impression
Taking that idea forward is a new range of profilometers. These instruments use the same 3D printer technology to scan the sclera using “structured light” rather than lasers and can produce an accurate digital profile of the eye which can, in one case, be transmitted directly to a CNC lathe to produce the finished lens.
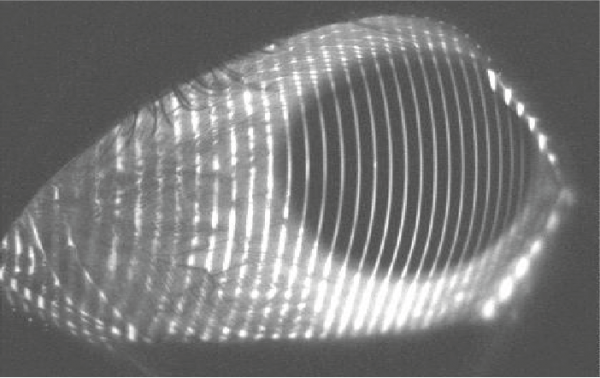
Figure 6: Structured light profiling eye surface
Summary
I can think of no previous time in the development of contact lenses that so much progress and knowledge have been attained over such a short timescale. From the development of lens designs going from simple C3 spherical lenses to fully customised, toric periphery multifocal bi‐torics in a decade.
This has coincided, of course, with the availabilities of instrumentation such as OCT, topography and more recently 3D profilometers.
The accuracy of modern manufacturing platforms which can be directly linked to digital imagery produced by this ever more sophisticated instrumentation will continue to develop this modality.
New materials are being produced to ensure that patients continue to benefit from this exciting addition to the specialist fitters armoury.

Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. Martin is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). He has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
More articles by Martin Conway:
