Orthokeratology for Soft Lens Dryness
By Martin Conway
Dryness and discomfort have long been quoted as one of the main reasons for patients struggling and/or dropping out of soft contact lens wear. Despite new materials, the dropout figures remain fairly constant.
In a clinically dry eye, the use of scleral lenses may protect the cornea from recurrent abrasions, and with or without the use of additional wetting drops, scleral lenses permit the cornea to be continually hydrated whilst contact with the lids and lens surface can be eliminated.
For the soft lens dropout, however, with an uncomplicated refractive error, the use of scleral lenses may seem an overly complicated remedy compared to the ease of use that they have been used to with frequent replacement or daily disposable lenses. The cosmetic wearer may not be sufficiently motivated to put up with additional cost and more complex insertion, removal procedures associated with scleral lenses.
Faced with a soft lens patient complaining of dryness and discomfort, the practitioner’s first thought may not always be to suggest orthokeratology. After all, if the patient is struggling with comfort with a soft lens, what chance will they have with a rigid gas permeable lens worn overnight?
A typical problem soft lens patient is a long-term wearer now reaching mid to late thirties who complains that they can no longer wear their lenses for the full working day as they once could. Dryness and irritation is exacerbated by air-conditioned offices and prolonged screen use. The environmental factors, combined with Visual Display Unit (VDU) use and a pre-presbyopic eye, should alert the practitioner as to what is to come. The increasingly frequent use of wetting drops may be accompanied by difficulties with vision due to the optical surface drying and permitting lipids to accumulate on the surface of the lens. Any residual astigmatism, previously tolerated, may also become an issue as amplitude of accommodation is lost, and yet the patient will be reluctant to wear spectacles as they have become accustomed to years of problem-free lens wear.
It is at this point that the ortho-k option should be introduced.
The ortho-k lens will be worn during sleep, newly-introduced hyper-Dk materials such as Optimum Infinite* permit rapid adaptation and the excellent wettable surface is not subject to dehydration. The sealed environment of the eye during sleep prevents evaporation.
The patient is used to contact lens wear, new insertion and removal techniques are easily learnt and, after a few days initial adaption, full vision is restored. The problematic working environment is no longer such an issue as the eye is not subject to lens wear during the working day.
Ortho-k is mainly used in children for managing the progression of myopia, and most academic studies have concentrated on this phenomenon. We forget, however, that originally it was developed as an alternative method of correcting refractive error and that myopia control application was a serendipitous side effect. The reason for the myopia controlling effect of ortho-k correction is the fact that central flattening of the cornea in ortho-k is accompanied by an equal and opposite steepening of the cornea at the edge of the treatment zone. This increased plus power is responsible for focussing the peripheral retinal image in front of the retina and thus reducing the elongation of the eye. In effect, the retinal image produced by an ortho-k correction behaves very much like a centre distance bifocal.
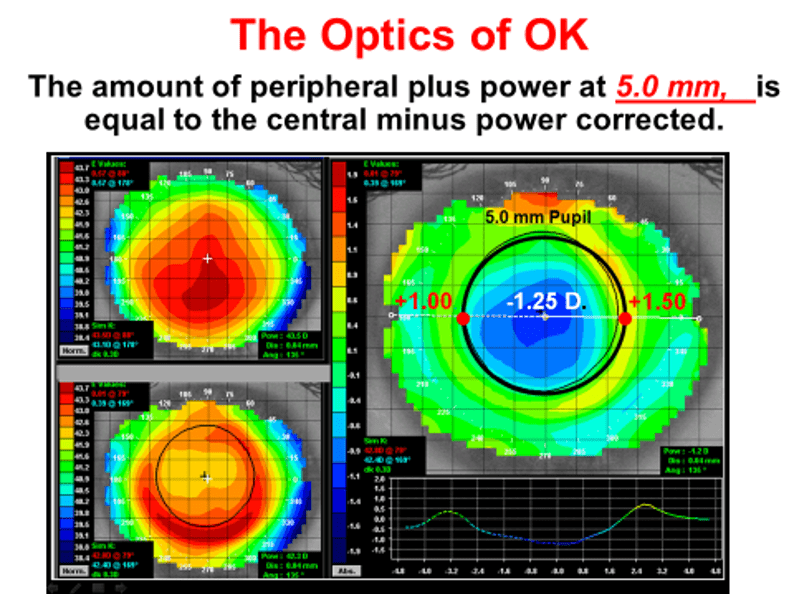
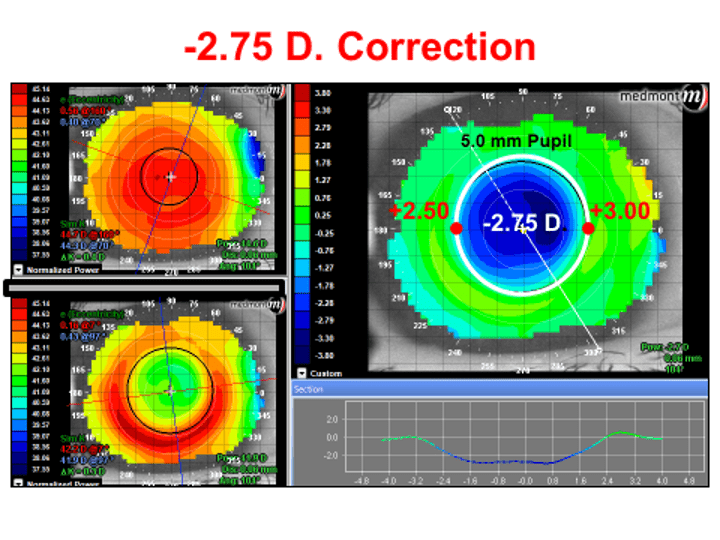
In the early presbyope described above, this centre-distance effect can also be harnessed to help the presbyope with near work. The amount of addition will depend upon the amount of correction.
As the patient ages, particularly with a low myope of around -1.25 say, then there will come a time when the required reading addition is higher than the normal ortho-k lens can produce. Ortho-k lens designs now exist which permit increased plus at the periphery to manage the increasing demands of the ageing presbyope.
It is easy for the practitioner to become blinkered into only considering a soft lens solution for a soft lens problem. Many patients who, having previously elected for soft lenses earlier in their lens wearing career, faced with difficulties caused by the modality would be more than willing to now try orthokeratology as a viable option.
Clinical studies have demonstrated that reduction in Goblet Cell Density occurs in soft lens wearers over time. These changes can be reversed when the patient switches to Ortho-k use.
Clinical Studies
One study (Carracedo et al, 2016.) ¹ looked at the effect of orthokeratology on two groups. One group were previously wearing silicone hydrogel lenses and the other group were non-wearers. The silicone hydrogel wearers showed a significant increase in Goblet Cell Density (GCD) and a reduction in dry eye symptoms after one month of ortho-k wear. (The baseline measurements were significantly lower for this group than for the non-wearers). The conclusion was that ortho-k may be a viable alternative for silicone hydrogel wearers with dry eye symptoms.
Another study (Luis H. Colorado et al, May 2016.)² looked at daily disposable hydrogel lens wearers over a six month period, and compared them with a control group who did not wear lenses over the period. This study showed that GCD was reduced in the contact lens wearers compared with non-wearers. Some of the contact lens wearers reported dry eye symptoms, and this group showed a 29% reduction in GCD, the other group of wearers had no symptoms, but still showed 13% reduction of GCD.
*Optimum Infinite is not FDA approved for overnight or extended wear.
1. Carracedo G, Martin-Gil A, Fonseca B, Pintor J. Effect of overnight orthokeratology on conjunctival goblet cells. Cont Lens Ant Eye.
2. Colorado LH, Alzahrani Y, Pritchard N, Efron N, Time Course Changes in Goblet Cell Density in Symptomatic and Asymptomatic Contact Lens Wearers. Invest Ophthalmol Vis Sci. 2016 May 1;57(6):2888–2894.

Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. Martin is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). He has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
More articles by Martin Conway:
Dry Eye and Scleral Lenses in Optimum
Salzmann’s Nodular Degeneration
The Evolution of Scleral Lens Fitting
