Scleral Lens Fitting Post-Refractive Keratotomy
by Luciano Bastos
Summary
Patient male, 46 years old, army official, history of post-refractive keratotomy OU performed in 1994, visual acuity was good until 2014 when it began to deteriorate. The patient had to retire early due to his condition and then began to practice law as an army lawyer. He had been wearing glasses which gave poor quality of vision and reduced acuity. He came to us from another state after visiting several doctors and testing different contact lenses in an attempt to improve his vision.
He was fitted with full scleral lenses and the results were an optimal fitting relationship, great comfort and excellent visual acuity while also preserving anterior eye and corneal physiological health.
Introduction
Our clinic has a long history of fitting irregular cornea conditions and since the early introduction of refractive radial keratotomy, many patients were referred to us in order to restore vision in cases where soft lenses or spectacles would not offer satisfactory results. During the early 90’s we relied upon the 12.7 mm wide RGP intra-limbal designs to provide the larger overall diameter to resolve cases like this. It was always a challenging process but our efforts did help many patients.
By 2014 we were able to utilise a full scleral lens design we developed after many years of research into the manufacturing and fitting of scleral lenses. My father, Dr Saul Bastos, MD asked me to study scleral lens technology and suggested that I contact his professor and friend Dr Perry Rosenthal, MD PhD (US) who became my mentor on the subject for years. I also relied on a great friend and specialist in the UK, Dr Ken Pullum FC Optom DipCLP.
During the first experimentations on manufacturing scleral lenses in 2006, we only were able to manufacture up to 16.0 mm. In the following years, new materials and diameters were available which allowed us to manufacture scleral lenses as large as 21.0 mm. There are some cases in which large, full scleral lenses are necessary, especially when there is a disease like dry eye or a large cornea with a large palpebral aperture.
In this case, we faced an irregular corneal condition with a large cornea and palpebral aperture which clearly needed a higher SAG and a wide landing zone. The fact that it was a post-surgical cornea that had been damaged by incisions and now had scars together with reduced mechanical strength due to damage to the collagen fibres also made me aware of the importance of oxygen delivery to the cornea. At the time of the fitting, we were working with the Optimum Extreme (125 DK) from Contamac, it was reassuring to be able to rely on a higher oxygen permeability as this case required full scleral lenses.
Examination
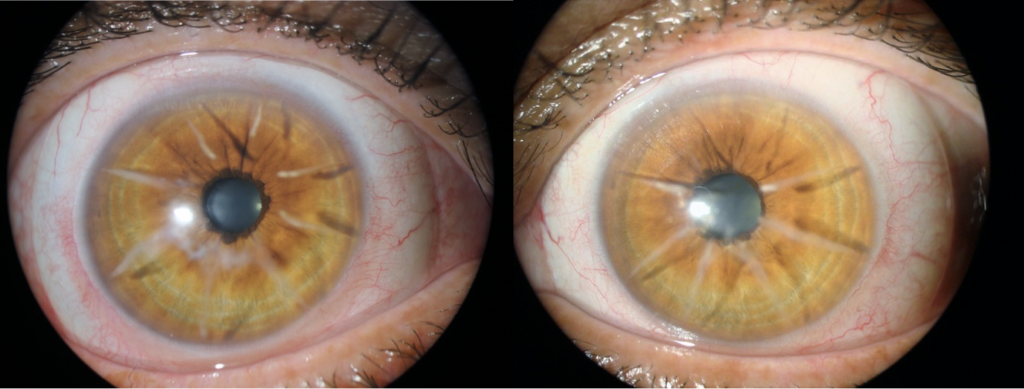
Biomicroscopy showed a series of eight radial incisions with significant depth OU and flatter topography at the central cornea. A decreased corneal thickness was also observed at the central and paracentral cornea. The slit-lamp cross-section view showed an abnormal corneal profile (Figures 1 to 4).
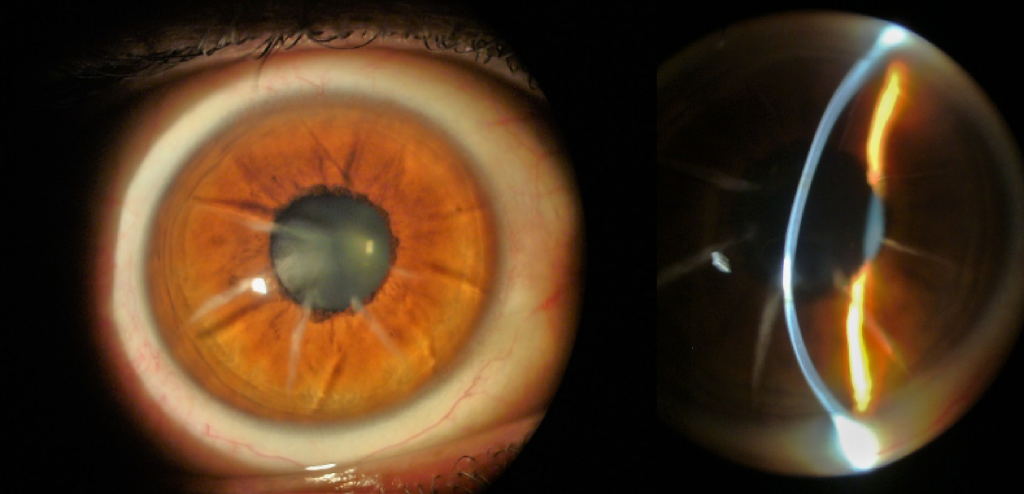
Figures 1 and 2: OD radial incisions and irregular cornea profile under slit-lamp.

Figures 3 and 4: OS radial incisions and irregular cornea profile under slit-lamp.
Endothelial cell count was lower than normal in both eyes, worst at OD, so we definitely would need a high Dk, a full scleral lens design and the system I developed called Wave Spline Technology (WST). WST is a ventilation channel system that allows tears to enter the fluid lens reservoir to help to deliver more oxygen to the cornea. We also performed a Pentacam Scan (Figures 5 and 6) and collected data from the precise maps this technology offers together with an OCT to verify each and every quadrant to optimise the landing haptic for a gentle and smooth fitting.
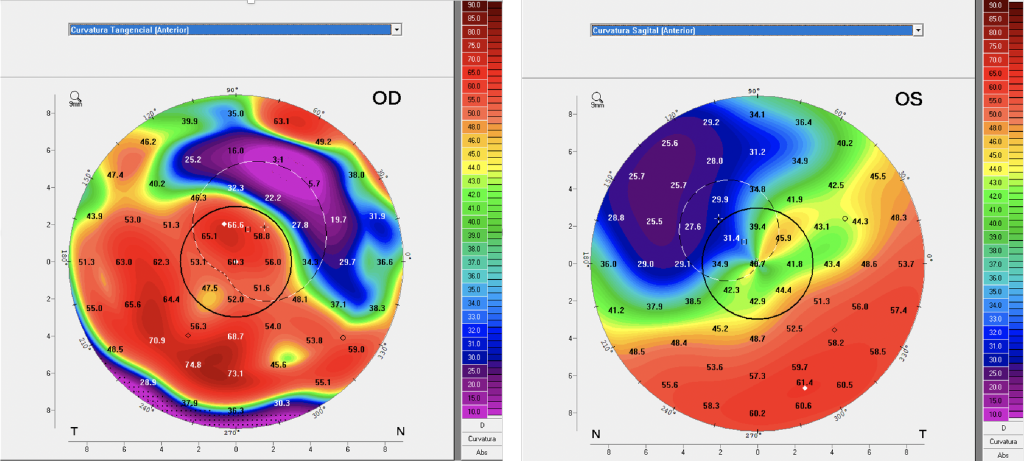
Figures 5 and 6: Anterior Sagittal Curvature large maps.
The patients that submitted to corneal refractive procedures were normally higher myopes and the larger amount of correction required necessitates deeper and more numerous incisions. Back in the day when this procedure was performed, the initial protocol was four radial incisions and, if additional correction was needed, an extra four radial incisions were made. I remember being in an ophthalmology congress with my father, Dr Saul Bastos, at which some surgeons were debating this technique and one of them said that he would perform a total of 12 or more incisions. That was really surprising to my father and me, as we were seeing those patients with those outcomes.
The procedure was abandoned with the advent of laser technology, which also has its complications. The reason I highlighted high myopia is that these patients should be carefully evaluated for glaucoma and retinal diseases as they are more prone to have posterior eye complications. Dr Marcelo Bittencourt MD (IOSB clinical director) examined the patient as a standard procedure with awareness that he was a high myopic patient before refractive surgery.
With the Density Average map from Pentacam (Figures 7 and 8), we can also observe the areas of the incisions (in black) with severe opacities. These areas also show the extensions of the incisions and its impact on the corneal epithelium and the corneal topography. The densitometer screening also helps to identify if corneal opacities or haze would change in subsequent examinations.
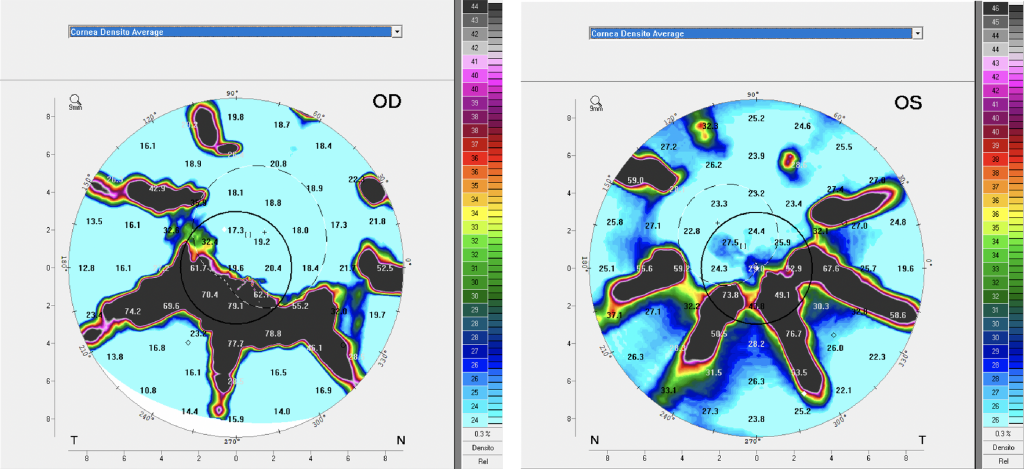
Figures 7 and 8: Density Average maps identifying opaque areas at the incisions.
The Scheimpflug and the 3D model images are also great tools to examine abnormal cornea conditions with high irregular astigmatism. The Scheimpflug is similar to the cross-section-view on the slit lamp but it can show the cross-section in different angles. The 3D cornea model is capable of giving a better comprehension of the overall aspect of the anterior cornea and also is capable of showing areas of opacities, it can be rotated in real-time so you can view it from different perspectives, (Figures 9 and 10).
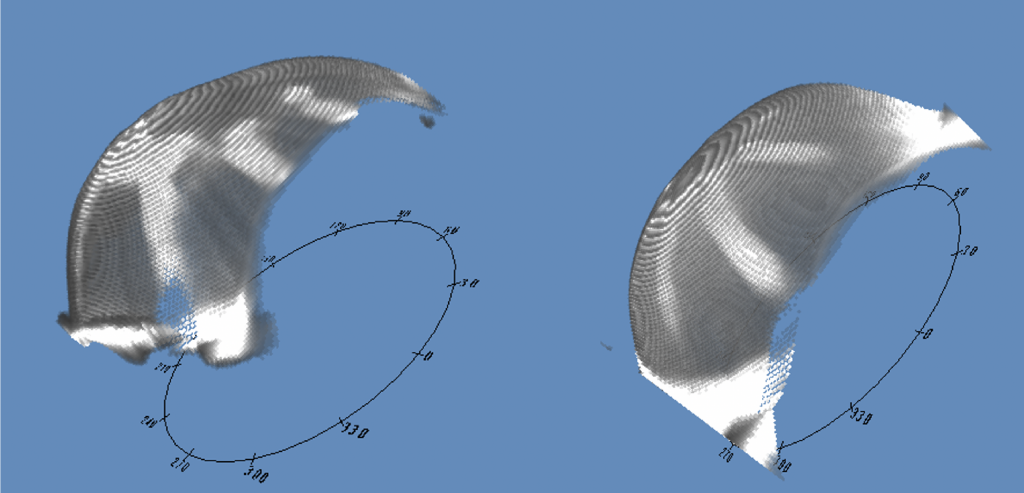
Figures 9 and 10: The 3D Corneal Model images from Pentacam, OD and OS.
We do not hesitate to use all the technology we have to get a comprehensive understanding of the case and data we can use to achieve the best possible speciality lens fit.
Contact Lens Examination and Fit Evaluation
This patient was fitted for the first time in 2014 with 19.6 mm scleral lenses. He wore the lenses for three years with no complications and came for a refit in 2017. Both fits were with the Optimum Extreme material (125 Dk).
In 2019, the patient came for a follow-up and I discussed the new Optimum Infinite material from Contamac that has a Dk of 180. The patient was happy to know more about it, and subsequently, he was refitted with the Optimum Infinite material. The lens parameters were:
| OD | OS | |
| BC | 47.50 x 45 (7.10 x 7.50) | 44.00 (7.67 mm) |
| Power | -15.00 | -8.50 |
| OAD | 19.6 mm | 19.6 mm |
| SAG | 7.711 | 7.270 |
| Material | Optimum Infinite | Optimum Infinite |
Figures 11 and 12 front images of the model SB Full Scleral lens, OD and OS.
Observe OD the enlarged opacity below the pupil, also visible in the density average map from Pentacam (Figures 7 and 11). The OS image (figure 12) also shows the visible incisions from the refractive keratotomy and it also can be compared to the Density Average image (figure 8) from Pentacam.
Initial thoughts were to design a reverse scleral lens design with a flatter posterior central base curve and a secondary, steeper base curve to overcome the flatter pattern at the central cornea. However, we were able to fit a double base curve, adjusting the base curve radius and optical zone diameters to achieve a good fit on OD as seen in figures 13 and 14.
At OS we designed a single base curve with a large optical zone diameter and we could overcome all the elevations on the cornea (Figures 15 and 16). Both eyes were fitted with a SAG that proved to be high enough after settling with four hours of lens wear. The frontal and cross-section view observed and the slit lamp shows the fluid lens reservoir at both perspectives.
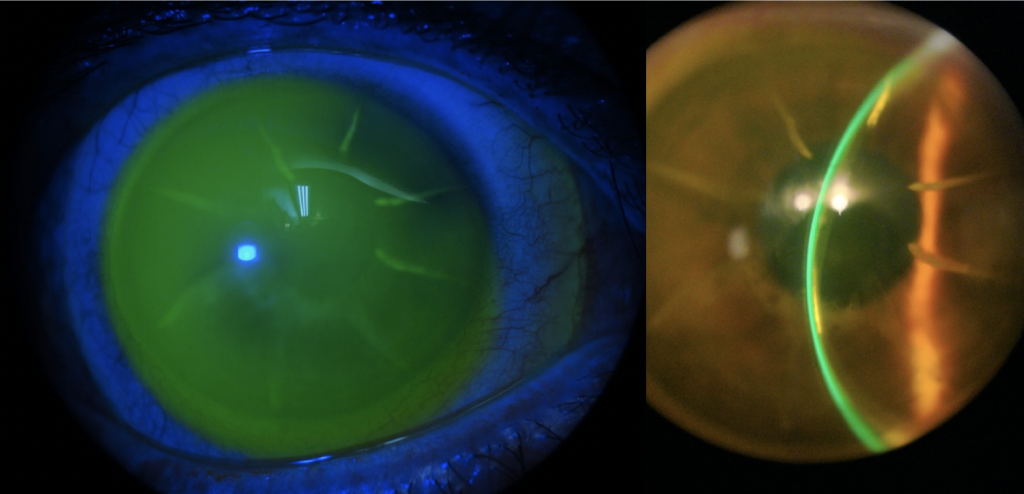
Figures 13 and 14: OD frontal and cross-section view on the slit lamp with fluorescein.
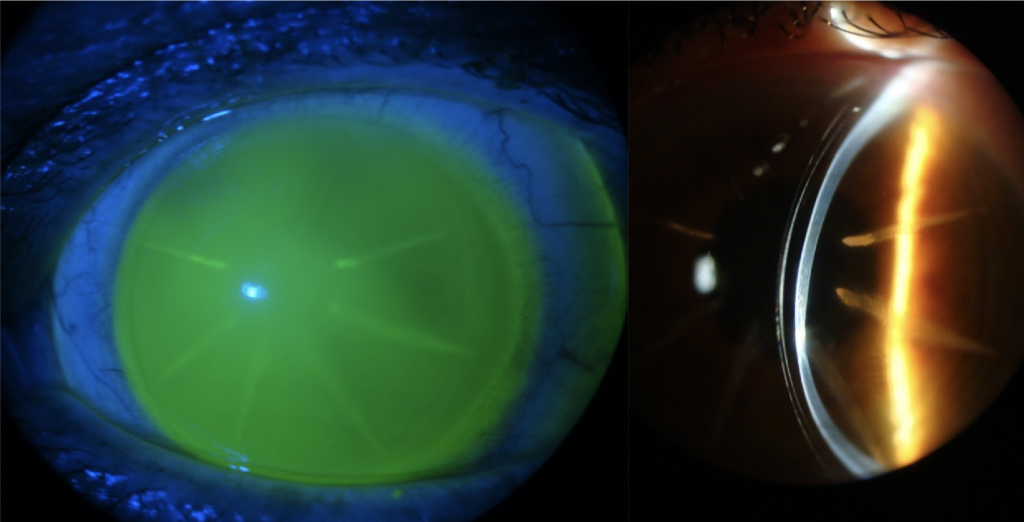
Figures 15 and 16: OS frontal view with fluorescein and cross-section view with white beam.
The patient was happy with the comfort, and visual acuity was 20/10 J1 OU. The visual outcome was much better than expected despite the fact he is 46 years old, (so he should be entering presbyopia soon) he was able to read J1 with no add correction. He was informed about the possible future need of add correction, we determined his dominant eye for possible near vision correction when necessary, utilizing reading glasses, monovision or a multifocal design in the early stages.
We also performed an OCT scan at eight different angles to have a better understanding of the landing pattern in each meridian. The scans were separated by each angle; one image of the limbal transition and the other of the landing haptic including the edge as you can see in figure 17.
The OCT exam is a great tool to identify areas where the haptic may present significant pressure over the conjunctival sclera, or excessive lift. With all information gathered from these 16 images generated by OCT we can plan and design the scleral lens with an estimation of toricity that we may apply to the haptic and align where required.
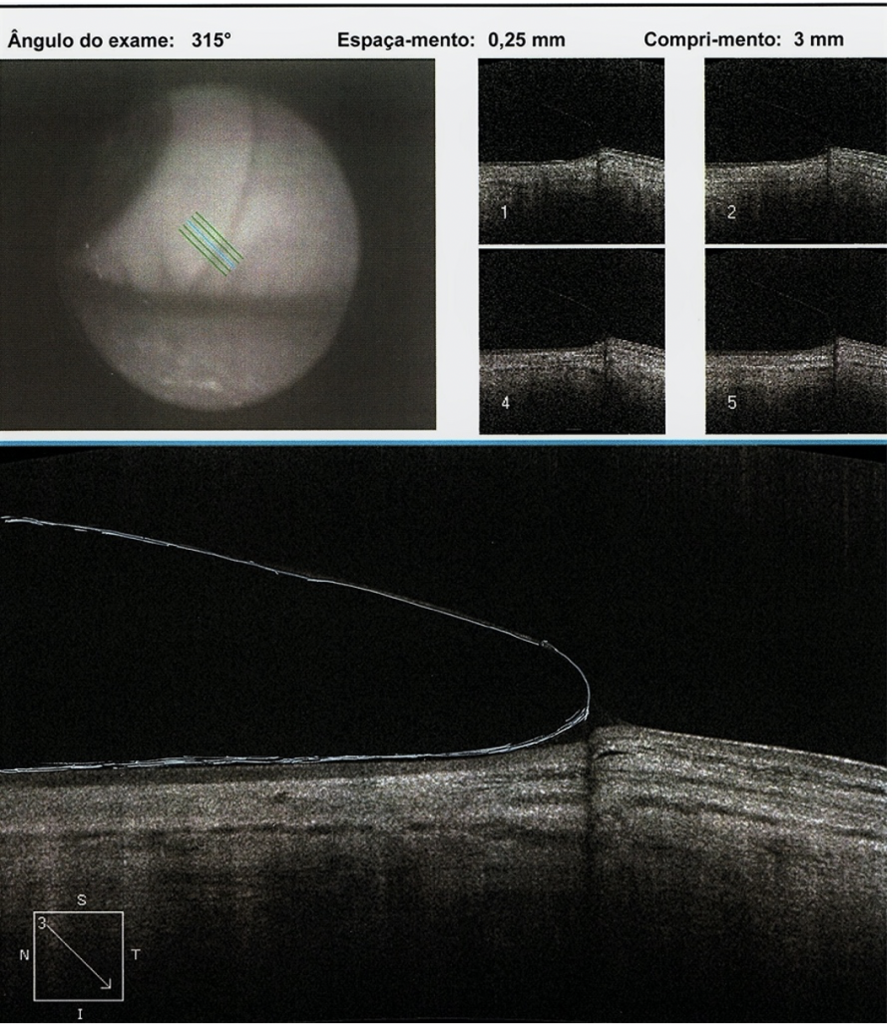
Figure 17: A single segment of the haptic showing scleral alignment.
Follow-up Visit After 120 Days
During the weeks following the dispense, the patient reported feeling good, with excellent vision. After about 120 days of dispensing, he was able to visit us again, bearing in mind he lives in another state.
Biomicroscopy during examination showed a crystal-clear cornea, specular biomicroscopy remained stable with a similar endothelial cell count. Visual acuity also remained stable and there was no sign of corneal edema or any complications. Our normal procedure during follow-up visits is to re-evaluate the fitting and consider what might be required to improve the overall fitting. In this case, we decided that with the next lenses we would increase the landing zone and also slightly augment the transitional limbal zone from the base curve to the haptic landing zone. This will allow the lens to have a better pattern over the limbus as it appears to be too close to the limbus (figures 13 and 15).
Customising the Scleral Lens Fitting
When we change any variable at the posterior curve, the optical zones and the overall diameter of the scleral lens SAG are affected. The more variables you change the more impact it has on SAG value, achieving a lower or a higher value depending on the changes made. If you have, like in this case, a SAG that you have as a reference it is a great starting point as you will need to apply the changes to customize the fitting. So, it is necessary to control these variables in a manner that the changes will result in a better fitting relationship while preserving the SAG value to a number close to the reference.
This is absolutely true with trial lenses as well; we always think about customizing the fit whenever it is necessary. If the practitioner does not have software to calculate these changes it is of utmost importance to have technical assistance from a lab consultant that may be able to provide the possible calculations to achieve the results the specialist wants. Another possibility is to use what Ultralentes call Digital Consultancy. In this case, the doctors are encouraged to produce frontal and cross-section view images through the slit-lamp and forward these photos or short videos to the lab. This is often the case as practitioners generally do not use contact lens software to design lenses. Ultralentes also provide the practitioners with a Consultancy Form that the doctor may fill and also make observations and drawings of the specific areas he wants to improve from the trial lens used.
Conclusion
The patient reported feeling really great with his new lenses, he mentioned that he was happy to change to a higher Dk material (Optimum Infinite). He reported greater comfort, visual acuity remained stable and the eye calm. The overall fitting was quite acceptable for a surgical cornea that has multiple incisions that had deteriorated the corneal physiology over the years.
We know that patient’s previous lenses were made in Optimum Extreme and were worn for two years, they were fine and the motive for a new fit was based on taking advantage of higher oxygen transmissibility rather than necessity. Although the lenses were still acceptable to wear, naturally, a new pair may impact visual quality as acuity had no change. What is important is that after four months of wearing the new material, the results were clinically excellent and the patient was happy with comfort and vision.
I also want to address that we had no problem manufacturing these full scleral lens designs in the Optimum Infinite material. It proved to be stable with excellent physical properties with a 180 Dk. This is really important especially when these speciality lens designs are planned.
At the time of writing this case, we already have several scleral lens fittings with Optimum Infinite and it is definitely a great and reliable material from Contamac. The higher Dk material for scleral lens patients means an extended wearing time but is especially important to post-surgery patients.
Here at the Instituto de Olhos Dr Saul Bastos (IOSB), 96% of the fittings are speciality RGP and scleral lens fittings. From these, about 70% are ectasic patients, including (most) keratoconus patients, pellucid Marginal Degeneration and keratoglobus. About 15% are post-surgical patients like post-penetrating keratoplasty (corneal transplants), post-radial keratotomy and post-laser surgery (Lasik and PRK), about 5% are dry eye patients. The remaining 10% of patients are moderate to high myopics, hyperopics, and aphakics. The introduction of the Optimum Infinite material is a great advantage to these post-surgery patients and those with the larger full scleral lens designs.
1. Banta JT. Ocular Trauma – Bascon Plamer Eye Institute. Miami, FL – Saunders Elsevier, 2007
2. Black CJ, Rosenthal P, Kaufman HE et al. Symposium on Contact Lenses. Transactions – New Orleans Academy of Opthalmology. St Louis: Mosby, 1973
3. Bowden TJ. Contact Lens: The Story – Cornwall, UK. London: Bower House, 2009
4. Cochet P, Amiard H. Contact Lens International Clinics. Boston: Little, Brown, 1969
5. Cvintal T, Munarin MAM, Moro F. Complicações do Transplante de Córnea. São Paulo, Santos, 2004
6. Duker JS, Macsal MS, Fontes BM. Anterior Segment – Rapid Diagnosis in Ophthalmology, St. Louis, Mosby Elsevier, 2008
7. Girard LJ, Soper JW, Gunn C. Corneal and Scleral Contact Lenses. Proceedings of the International Congress. St. Louis: Mosby, 1967
8. Girard LJ, Soper JW, Sampson WG. Corneal Contact Lenses. St. Louis: Mosby Co. 1970
9. Godinho C, Dantas B, Sobrinho M.et al. O Padrão CG em Lentes de Contato. Bastos, L. Cultura Médica;. pág. 301 a 313. 2010
10. Jenkin L, Tyler-Jones R. Theory and Practice of Contact Lens Fitting: Hatton Press 1969
11. Pena A. Bastos, S et all, Clínica de Lentes de Contato. Cultura Médica, 1989; pág. 69-79
12. Philips AJ, Speedwell L, Morris J. Contact Lenses – 5th ed. Ed Butterworth Heinmann Elsevier 2007
13. Ferrara, Paulo. Anel de Ferrara – Cultura Médica – 2006
14. Romero-Rangel T, Stavrou P, Cotter J et all. Gas Permeable Ocular Prosthesis Therapy in Ocular Surface Disease. Am J Ophthalmology, 2000, 130: 25-32
15. Rosenthal P, Cotter JM, Treatment of Persistent Epithelial Defect with extended wear of a fluid-ventilated gas permeable scleral contact lens Am J, Opthalm 2000; 130: 25-32
16. Rosenthal P., Cotter JM. The Boston Ocular Surface Prosthesis in the management of Severe Ocular Surface Disease. In: Foulks G. (ed.) Ophthalm Clin A Am 2003; 16: 89-93
17. Schein OD, Rosenthal P, Ducharme C. A Gas Permeable Scleral Lens for visual rehabilitation. Am J Ophthalmol, 1990; 109:318
18. Fadel, Daddi DOptom, FSLS, FBCLA, FAAO – Scleral Lens Issues and Complications: Their Recognition, Etiology and Management. – Dougmar Publishing Group Inc. August 2020
Thank you to Dr Luciano Bastos for contributing to Global Insight.

Mr. Bastos is the director and clinical instructor of specialty contact lenses at the Instituto de Olhos Dr. Saul Bastos (IOSB), and is the director and specialty lens consultant of Ultralentes, a small laboratory specializing in GP and scleral lens designs in Porto Alegre, RS, Brazil.
More from Luciano Bastos:
