Conjunctival Scarring Case Report
By Martin Conway
Conjunctival Scarring
Many conditions can cause the conjunctiva, the thin transparent membrane that covers the white of the eye and the underside of the eyelids, to become scarred. Scarring damages the conjunctiva and prevents it retaining the protective mucous layer, which helps tears adhere to the surface. Patients may have symptoms of dry eye, with grittiness, burning and in severe cases, loss of vision due corneal tissue loss.
On a global scale, a major cause of conjunctival scarring and blindness an infectious disease called trachoma, which is not common in temperate climates but affects millions of people in North Africa and South Asia.
Cicatrising Conjunctivitis
The term “ cicatrising” means scarring, but is generally reserved for scarring where there is significant tissue shrinkage, usually with distortion of the fornices and/or lids.
There are many causes of scarring: Trauma, Surgery, Infectious Conjunctivitis (Rare), Allergy (Vernal or Atopic Keratoconjunctivitis), can all induce scarring.
Severity can vary from trivial to sight threatening.
Pharmacological Treatments
A variety of pharmacological treatment may be used; artificial tears and ointments to aid lubrication, as well as topical or systemic immunosuppression if of autoimmune aetiology. Conjunctival or buccal mucous membrane grafts, stem cell transplantation, amniotic membrane transplantation and lid surgery are possible ophthalmological interventions.
Therapeutic Contact Lenses
All types of lenses have been used, but the lens of choice for a particularly dry eye is a scleral lens.
Case Study: Atopic keratoconjunctivitis with conjunctival cicatrisation
Practitioner: Mark Darling UK.
Patient: Ms S Female Age: 38

History: Ms S had vernal keratoconjunctivitis as a child and now has atopic keratoconjunctivitis with secondary ocular surface failure, due to chronic inflammation. She is dependent on topical steroids to control ocular inflammation and discomfort, together with a range of lubricants, vitamin A ointment and other medication as necessary, when her eyes are severely inflamed.
Unaided acuity was 6/60 improving to 6/24 with pinhole in the right eye, and 6/24 improving to 6/18 with pinhole in the left.
Tear production is healthy, although the right upper tarsal plate showed severe cobblestone papillae. The left upper tarsus is less affected. Cicatrisation (scarring) is present in both eyes and the fornix depths are reduced in all four eyelids. She has ocular surface failure in both eyes (R>L), with diffuse punctate epitheliopathy and corneal vascularisation.
Scleral Lens Fitting: Ms S was originally fitted with SoClear lenses some 5 years ago. These improved vision and comfort, but tended to move excessively. She was then, refitted with a larger design (17mm) by another practitioner about one year before her visit to Mark Darling’s practice. The larger diameter had not solved the problem. Ms S said that the lens “clicked” as she blinked. Slit lamp examination showed significant debris collecting under the lens as it moved under the action of the blink, causing discomfort and inflammation.
Initially a conventional 16mm design was tried, but again it tended to move excessively. Mark concluded that the excessive movement was probably caused by the increased traction between the scarring on the upper tarsal plate and the front surface of the lens.
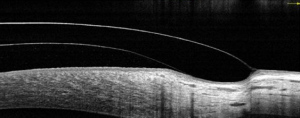
Mark had recently taken delivery of a new lens design , Comfort 15 from No 7 Contact Lenses, in Optimum Extra. This is a 15mm lens with a design offering limbal clearance and a relatively small scleral footprint.
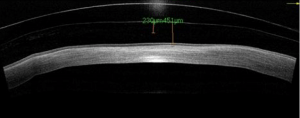
A stable and comfortable fit was eventually obtained by using a steeper central clearance than is normally advised and acuities of R 6/12 L 6/9.5 were obtained. No blanching of vessels occurred, despite the apparent compression of the landing zone. A sealed and stable fit was obtained and the higher clearance did not affect the acuities.
Lenses Dispensed:
R 7.80/15.0 +1.75 L 7.70/15.0 +0.75/-1.50 x 155
(LE front surface toric with prism stabilisation.)
Comfort 15 lenses, No7 Contact Lenses in Optimum Extra
The increasing availability of designs using a variety of fitting philosophies, enable practitioners to now have a number of options available to them when confronted by patients with more challenging conditions.

Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. Martin is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). He has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
More articles by Martin Conway:

