An Update on Scleral Lenses
By Martin Conway
Scleral lens use has been growing steadily over the past decade, driven mainly by the U.S. market where scleral fitting has dominated discussions in clinical publications for the past four years or more. This growth in usage has been matched by the growth in laboratories offering scleral lens designs. Once the province of a few specialist manufacturers, most laboratories now offer a design, either of their own, or licensed from a foreign manufacturer.
I can think of no previous occasion when the profession’s top researchers from all over the globe, but in particular the United States, all shared a specific focus on a single modality. This concentration of minds has resulted in a rapid accumulation of knowledge that has resulted in novel designs that are almost immediately available to the practitioner.
The reason for this meteoric rise in popularity has a lot to do with the fact that the scleral lens offers huge advantages to practitioners, laboratories and, most importantly, to patients. Patients with difficult, irregular corneae or dry eyes can now achieve visual acuities normally only obtained with a corneal GP lens, yet with comfort levels associated with soft lenses or, in some cases, even greater. Laboratories can command higher prices that practitioners can pass on to patients prepared to pay for the life-changing benefits that this modality can offer. All without the fear that the internet is going to undermine their investment.
There are some issues yet to be resolved however, and any practitioner thinking of introducing sclerals to their practice should be aware of them.
Scleral Shape
Our previous knowledge of scleral shape has proven to have been incomplete. Increased research effort, coupled with advances in technology has gone a long way to improving that position.
We now know that the sclera shape is not what we once thought of as a clearly delineated curve, separate from the limbus. OCT imaging shows a contiguous line of tissue with little change of curvature. Little was known of the shape of the sclera beyond the immediate limbal area but recent research using a new wide-field topographer has explained what some of had been beginning to suspect. The traditional spherical shape of conventional sclerals may need to be rethought. This research conducted by members of the Scleral Lens Shape Study Group¹ (SLSSG) used data collected at 14. 15 and 16mm from corneal centre to classify scleral shape into four groups as shown below.
Scleral Surface Patterns Observed in 140 Scleral Lens Patients
| Group | Pattern Description | N% |
| 1 | Spherical | 8 (5.7%) |
| 2 | Toric-Regular | 40 (28.6%) |
| 3 | Asymmetric High or Low Points | 57 (40.7%) |
| 4 | Periodicity different from 180º | 35 (25%) |
It would suggest that a spherical periphery is only really suitable in under 6% of cases and 70%+ of eyes would be better served with a toric periphery, and some might even need a more complex design still. Many practitioners who have been fitting sclerals for some time had come to this conclusion on their own, and labs are reporting usage of toric peripheries in as much as 70% of new fits. This ties neatly into the figures from the research. Many labs are now incorporating this feature as standard in their fitting set lenses.
Fogging
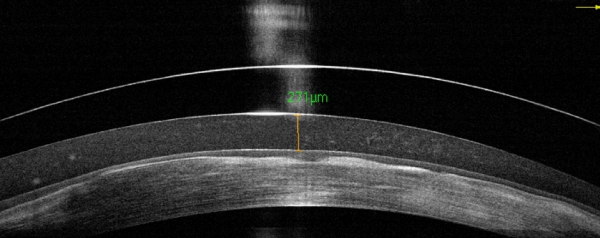
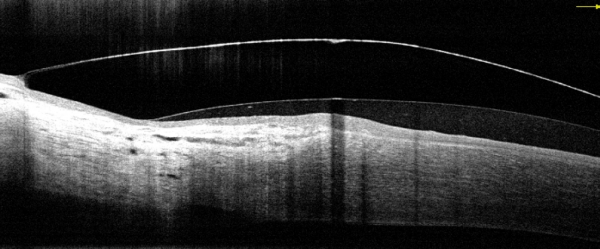
These findings may go some way to explain a phenomenon peculiar to sclerals – “Mid-day Fogging” as it is known has been an annoying feature for some wearers. After a few hours wear the tear film becomes increasingly cloudy until the patient needs to take off the lens, rinse, replace the insertion fluid and reinsert the lens to maintain clear vision. The following images are of a patient I saw recently:
Instilling Fluorescein into the eye without removing the lens soon identifies to source of the problem.
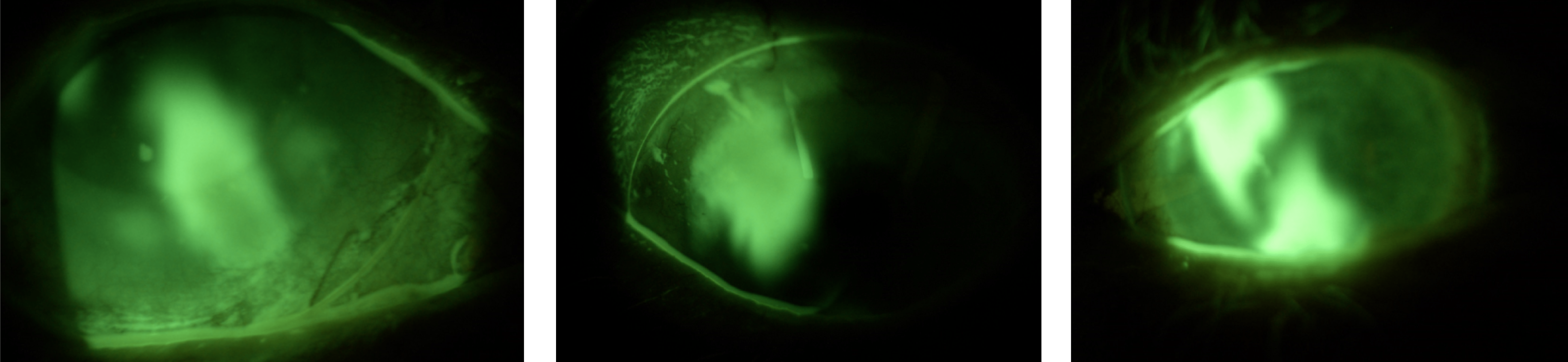
| Fig 1 | Fig 2 | Fig 3 |
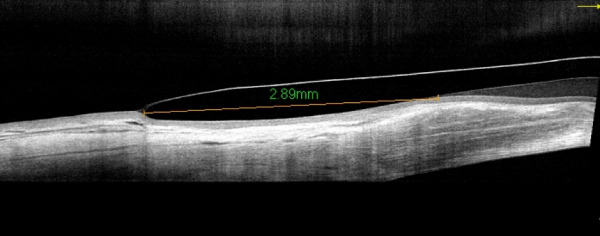
Within seconds of instilling Fluorescein, the dye encroaches under the lens at 5 and 11 o’clock ( Figs 1 and 2). Within minutes the two plumes of dye have merged in Fig 3. A scleral lens should be a sealed system. Once initial settling has occurred, it should be impossible for contaminants to enter the post-lens tear reservoir. In this case, although the lens was fitting well along the 180 meridian, it was rocking under the influence of the blink to pump lipids under the lens and form the suspension seen in the OCT image above. In extreme cases, edge standoff can result in conjunctival prolapse, where a conjunctival flap is sucked up under the lens by the suction caused by the lens rocking. In more subtle cases, the incomplete seal is barely noticeable through the slit lamp, but is sufficient to allow lipids to enter under the lens and cause fogging.
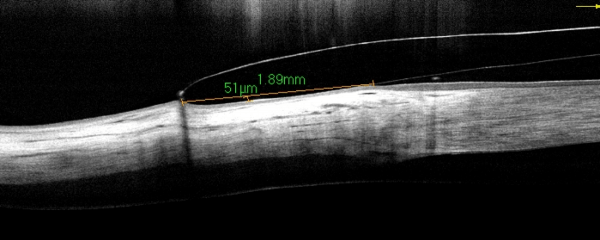
Refitting the lens with a toric periphery and reducing the central clearance by 100 microns solved the problem.
OCT Imaging
Traditionally, scleral lenses are fitted using fluorescein and observing the thickness of the tear layer through a narrow slit lamp beam at 45° to the eyepiece. The vault is assessed by comparing the thickness of the film to the known thickness of the trial lens. This method is subject to error however, and the greater availability of OCT imaging in practice now permits a much more accurate measurement of clearances and permits
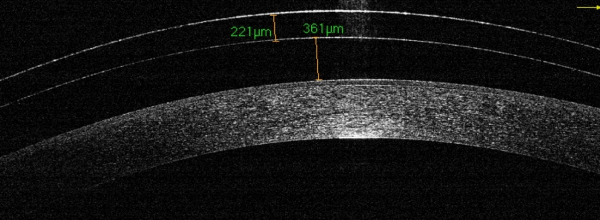
As with most other lens types the secret of a comfortable lens lies in the design and the alignment of the edge. The OCT permits the practitioner to view the edge profile in detail. Not all lenses are the same!
Dk and Scleral Lenses
Whilst there is little doubt that scleral lenses are here to stay, we should still be mindful of the fact that today’s lenses are made from traditional GP materials that were designed for use in corneal lenses that are half the thickness of a scleral. This, combined with the fact that the tear layer has a Dk of around 80 means that we are significantly reducing the amount of oxygen passing through the lens/tear combination when compared to a corneal lens. On top of this, the scleral lens does not benefit from the tear pump action to replenish the tear reservoir – it is effectively a sealed system.
Most of the work done on this subject is based upon mathematical modelling and suggestions of minima for Dk and lens clearances are all therefore theoretical. Clinical observations are suggesting that other mechanisms may be at work that are supplementing the oxygen supply beyond the mathematical model’s restrictions.
This may have something to do with the fact that the mathematical model treats the tear layer as another lens, where in fact it is a fluid. Mixing of the tear lens layer occurs during the blink as we have seen with the fluorescein images above, and this may well assist the passage of dissolved oxygen through that layer and boost the eventual amount of oxygen reaching the cornea.
Conclusion
Sclerals are exciting interest around the world and are offering solutions for many patients, some of whom have struggled for years. There are still some unanswered questions however, and that is part of what makes this modality so intriguing. There is no doubt that we will learn more as we progress. The use of new instrumentation will make fitting more precise, and designs will improve to eliminate fogging and other issues. In the meantime many patients are now reaping the benefit of the recent whirlwind development of this exciting market development.
Thank you to Tom Arnold OD, FSLS, Owner & Optometrist, Today’s Vision Sugar Land, P.A for contributing the feature imagery to this article.
1. DeNaeyer G, Sanders D, van der Worp E, Jedlicka J, Michaud L, Morrison S. Qualitative Assessment of Scleral Shape Patterns Using a New Wide Field Ocular Surface Elevation Topographer. JCLRS [Internet]. 16Nov.2017 [cited 30May2018];1(1):12-. Available from: http://www.jclrs.org/index.php/JCLRS/article/view/11

Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. Martin is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). He has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
More articles by Martin Conway:
