Ortho-k and the Emerging Myopic Child
By Martin Conway, Dr Artur Khasanov and Aigul Esmukhambetova
Introduction
Whilst orthokeratology (ortho-k) was originally used as an alternative to spectacles and regular contact lenses and is still a viable option for those candidates, it is used these days predominantly for the management of the progression of myopia in children.
A by-product of compressing the central zone of the cornea in order to correct the existing myopia is that the periphery of the optic zone receives a relative increase in plus power equal to the minus power produced in the centre.
A myope with a correction of -1.00Dioptres (D) will therefore have a +1.00D addition at the periphery of the treatment zone. Likewise, a -3.00D treatment will benefit from +3.00D at the periphery. It is this unintended side effect that gives an ortho-k correction it’s beneficial effect for the young myope.
Early studies, looking at the effectivity of standard ortho-k using standard lens designs produced varied results:
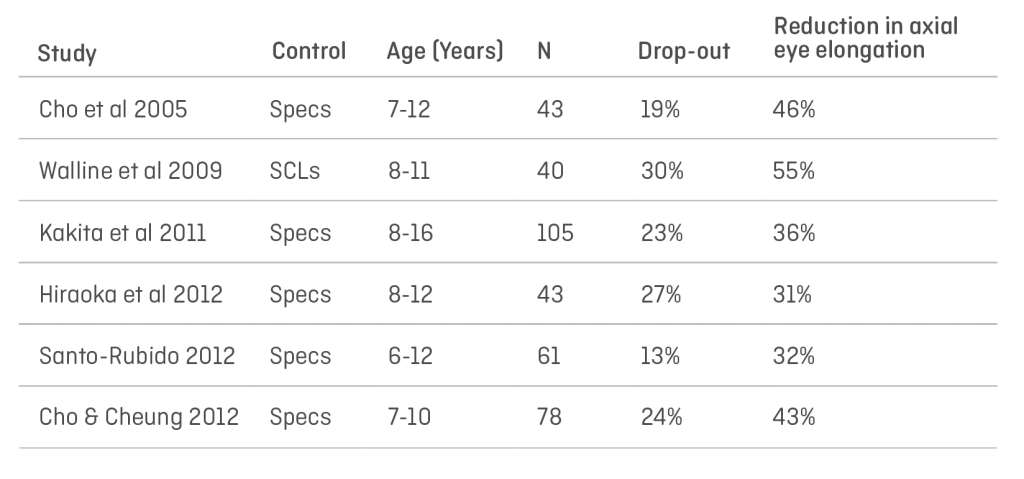
The studies all used standard lens designs approved within the various jurisdictions where they were conducted. Spherical equivalent powers were between -1.00D and -5.00D, and therefore the plus power achieved at the periphery varied accordingly as a result. It is my contention that this variation in results was produced by the mix of prescriptions within the individual cohorts – those with higher a proportion of high myopes benefitted from higher plus in the peripheries of those treatment zones and therefore more effective reduction in axial growth.
We are no longer constrained by fixed designs, lens design software packages are now available from a variety of sources that will allow the practitioner to have greater control over the prescribed lens for the individual patient’s needs.
The following case study was kindly prepared by Dr Artur Khasanov, eye care practitioner and owner of “Tochnaya Optika Lab”, Orenburg, together with Aigul Esmukhambetova, optometrist, and clearly demonstrates that increased plus power has a greater effect on the slowing of myopic progression in low myopes than conventional ortho-k designs.
Clinical observations of patients, users of Ortho-K lenses
Patient S., 17 years old. He first contacted us in 2014, at the age of 11.
Visual acuity at the time of the visit to a doctor:
OD 0.4 -1.50. = 1.2
OS 0.3 -1.75 = 1.2
The patient was fitted with Ortho-k lenses. We used ortho-k lenses available at that time in our market. Visual acuity while wearing ortho-k lenses:
Visus 0.8 both eyes.
Visual acuity in 2016:
OD 0.1 -2.75 = 1.2
OS 0.1 -2.75 =. 1.2
For two years of using ortho-k lenses (from 2014 to 2016), the progression of myopia was 1.25 D in the right eye and 1.00 D in the left eye.
At that point, we had the opportunity to independently calculate custom-made ortho-k lenses and decided to fit this patient with them.
Visual acuity after fitting: visus OD and OS = 1.2
Since 2016 to date, there has been no myopia progression and the patient continues wearing custom ortho-k lenses.
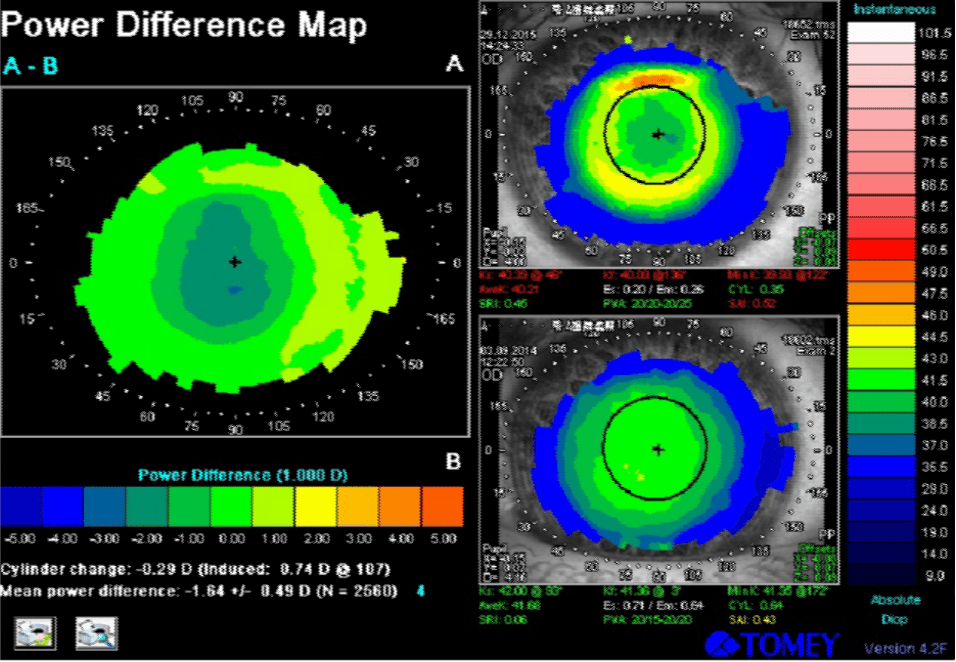
Below are corneal topography images of the right and the left eye during the first lens wear. The tangential power difference map shows that the ring in the projection of the reverse zone is green-yellow. This means that in patients with a low level of myopia it is impossible to achieve a significant myopic defocus on the periphery of the retina. It is in these patients that we observe a more pronounced progression of myopia than in patients with medium and high degrees of myopia.
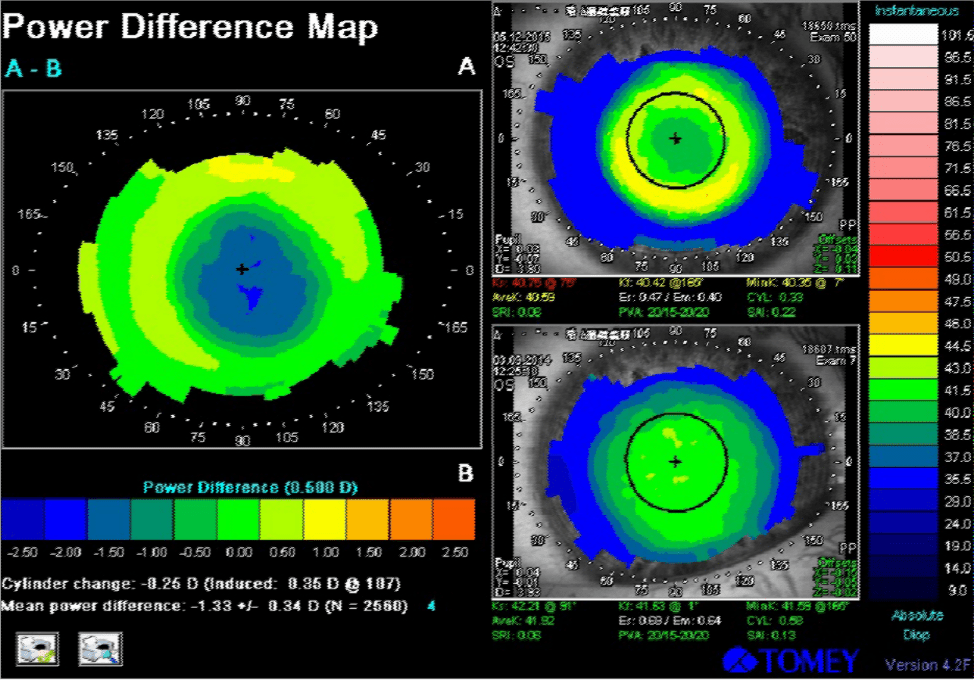
Below are corneal topography images of the same patient, while wearing customised lenses.
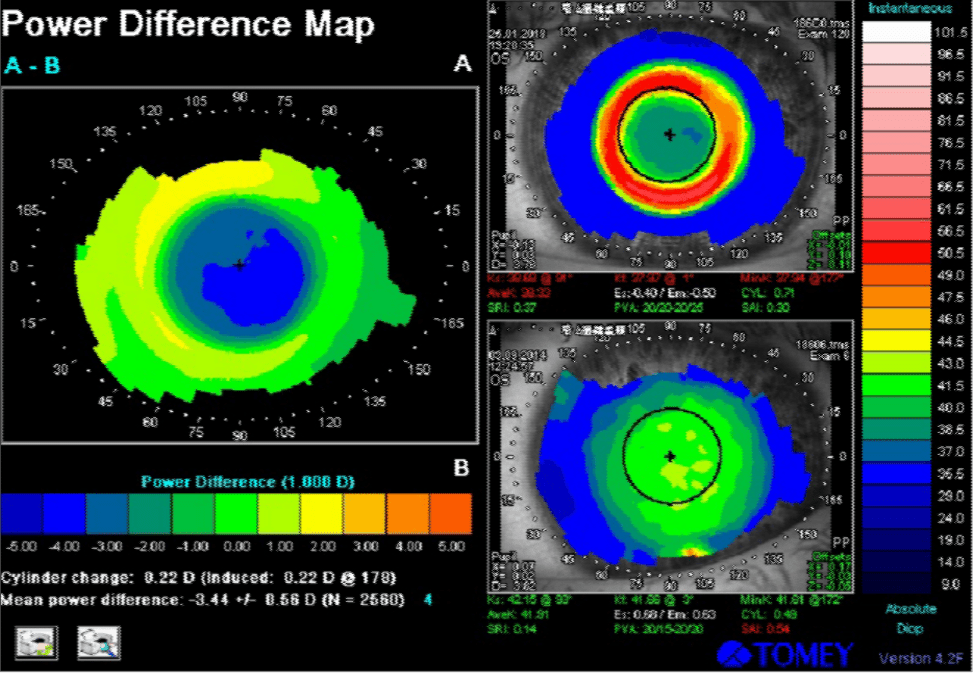
On the corneal topography image, the ring turned red, which means that in the projection of this zone the cornea has become “steeper” and has a high refractive power. We managed to increase the “+” in the projection of the pupil edge and thus achieve a pronounced peripheral myopic defocus.
This was achieved by increasing the tear lens clearance in the lens’ reverse zone. We used increased compression factor and asphericity of the back optic zone. According to our observations, to stabilize myopia, we need to achieve a clearance of at least 80 microns.
Conclusion
Obviously, this is just one example, but results such as these are being found around the globe and are pointing to the fact that “traditional” ortho-k designs may not be exerting sufficient forward movement in the peripheral retinal image shell in lower myopes than is required to achieve the optimal effect on the growth of myopia. This means that for the child with a -1.00D prescription, they will progress, albeit more slowly, until their prescription is such that sufficient peripheral power in the periphery is reached.
More research is needed to establish what the “sweet spot” is, but in the meantime, practitioners may wish to look at what options are available from their laboratories to increase the plus effect in the periphery for these patients.
The Future
Existing lathes are capable of producing these designs as Dr Khasanov’s case study demonstrates. More research is needed to establish whether there is a standard minimum amount of plus power in the periphery required to achieve this stabilising effect or whether an algorithm will be necessary to calculate the optimal lens design for each patient taking into account refraction, both peripheral and central, pupil size, etc.
We are now told to use the term Myopia “Management” rather than “Control” as we cannot accurately predict the outcome of these treatments. Lens design improvements such as outlined above, coupled with developments in instrumentation to monitor progress and amend designs accordingly should mean that we may soon achieve true control of this growing problem.
Thank you to Dr Artur Khasanov and Aigul Esmukhambetova for contributing to Global Insight.
Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. Martin is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). He has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
More articles by Martin Conway:
Every Cloud Has a Silver Lining
Orthokeratology for Soft Lens Dryness
Dry Eye and Scleral Lenses in Optimum
Aigul has been working with the ophthalmologist since 2008. In 2013 she qualified as an optometrist. Aigul specialises in fitting any types of contact lenses.
Related Case Studies:

Artur graduated from Orenburg State Medical Academy in 1995. He has been working as an ophthalmologist since 1996. Artur specialises in fitting any types of contact lenses. In 2019 he opened a laboratory for contact lens manufacturing in Orenburg.
