Severe Case of Corneal Abscess in a Patient with Acute Keratoconus
Doctor, my eye has a spot.
by Marcela Soria, OTC
Introduction
Serious Ocular Surface Disease (OSD) encompasses a variety of conditions that significantly affect a patient’s quality of life. This is often secondary to a primary systemic condition, in which case a patient will have other associated health problems. OSD directly affects the patient’s daily life, reducing their ability to work, study and exercise, as well as having an effect on their leisure and social life. These patients are often depressed and hopeless when traditional management strategies have failed.
In many cases, it is necessary to protect the cornea to aid in its healing due to serious injuries and in treatment for tissue recovery with loss of transparency, such is the case that I present below, where the patient appeared at my office stating that, his wife insisted on seeing me due to “having a spot on his eye”.
Patient History: Evolution of the Case
38-year-old male patient suffers from bilateral keratoconus and used RGP contact lenses 19 years ago with excellent tolerance and visual acuity.
On his previous visit, his topography and pachymetry studies showed signs of weight loss and some stretch marks in OD. The patient was referred to his ophthalmologist and it was suggested to change the modality of his contact lenses.
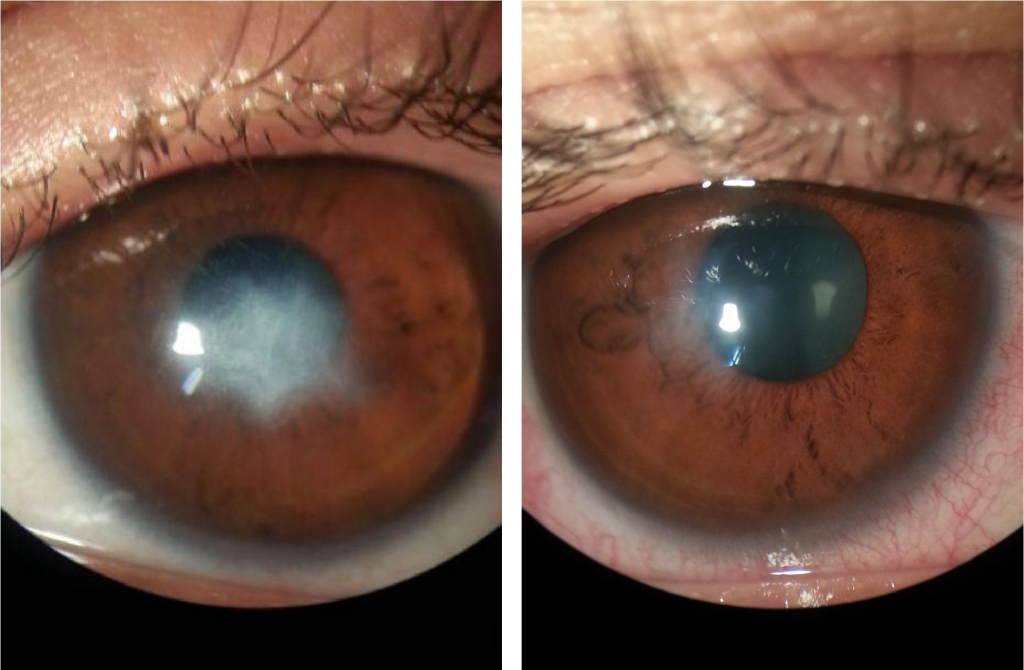
Two years passed until the fateful day that he visits my practice with the “spot” on his eye. The diagnosis was a severe corneal abscess – remarkably, the patient did not feel pain!
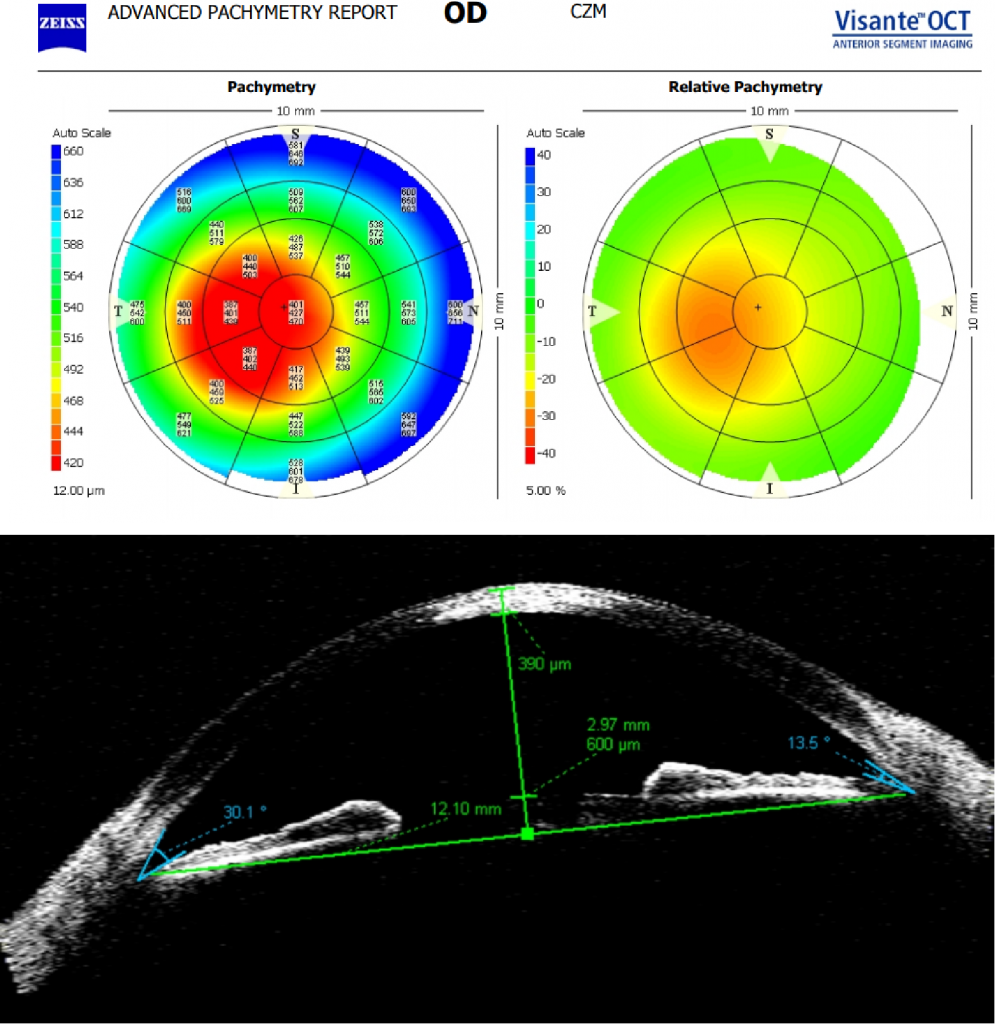
- Pachymetry and Visante OCT current OD: central thickness min 401, and max 470 (below).
- Keratometric data OD 49.50 x 58.75 symmetric oval keratoconus.
- VA 1/10 with glasses and 9/10 with contact lenses prior to injury, reduced to 4/10 with central leukoma.
Treatment
The patient’s treatment plan included scleral lenses and a substitute reservoir with autologous serum alternating with hyperosmolar saline and topical treatment with antibiotics, anti-inflammatories and cell regenerants. Additionally, the patient was instructed to use a moisturising gel at night, without contact lenses.
In addition to loss of vision due to keratoconus, and because the “spot” occupied 2/3 of his cornea, the patient could not continue with his activities wearing glasses due to his low visual acuity. Rehabilitation with contact lenses was absolutely necessary during topical treatment with antibiotics and anti-inflammatory drugs with corticosteroids.
An ESCLERA lens (Mediphacos) with a diameter of 16.5 mm and a toric haptic was manufactured. Taking into consideration both the patient’s corneal irregularity and the toricity of the sclera, the lens was made in Optimum Infinite material by Contamac, with a Dk of 180 and a central thickness of 270 microns to ensure oxygenation.
Scleral Lenses
Scleral lenses can be used for persistent refractory epithelial defects. These lenses vault over the cornea to protect the ocular surface and provide a reservoir for hydration. Patients who have severe ocular surface disease may benefit significantly from the use of scleral lenses, although they have not been specifically recommended for a scleral lens evaluation.
In these cases, the scleral lens fulfils a therapeutic bandage function and contains a liquid reservoir that protects the cornea, helps in its treatment and subsequent recovery.
Autologous Serum
Autologous serum drops have been reported as beneficial in the treatment of persistent epithelial defect over conventional therapy. The patient’s serum is diluted to a concentration of 20% and the drops are used inside the reservoir of the scleral lens. The therapeutic effect is promoted by various growth factors contained in the serum, including vitamin A and immunoglobulins.
Although most studies, as well as clinical experience, have shown favourable results with autologous serum, several factors limit its use in clinical practice. These include the cost, the need for blood collection and the lack of familiarity with this approach among doctors. Further, it is essential to have the support of an interdisciplinary team to closely monitor the evolution of the tissues, and the patient must be aware and strictly follow the instructions of the professionals involved.
Conclusion
The use of autologous serum on ocular surfaces with persistent damage has been shown to be beneficial and effective for tissue recovery. The patient quickly recovered visual function, including corneal transparency. Furthermore, autologous serum treatment presents low risk, with immunologic incompatibility as the main side effect.
Although not a cure, scleral lenses can often significantly reduce symptoms in some patients and improve vision to the point that they can resume activities that they previously enjoyed. Work in interdisciplinary teams is essential to obtain the best results.
Offering the patient everything that is at our disposal, with knowledge and awareness of the use of these new technologies, is what really makes the difference in the improvement of the patients quality of life.
Thank you to Marcella Soria for contributing to Global Insight.

Owner and Consulting Manager of LuxAR Argentina, Marcela Soria has been a contact lens optician since 1990. She is a member of the Scleral Lens Education Society and specialises in customised lenses for keratoconus and irregular corneas. Currently, she is a consultant and laboratory researcher for Mediphacos Brasil in the development of new products for irregular corneas and dry eye.
