Goodbye Keratometers, Hello Topographers
by Nick Howard
A reflection on the limitations of keratometry and the advantages of topography in modern day contact lens fitting
Introduction
Portuguese Ophthalmologist Antonio Placido’s remarkable invention in 18801 almost revolutionised methods of measuring ocular surface shape. The inventive and imaginative scientists of the Victorian era provided the world with some truly breath-taking adaptations of cutting-edge technologies available in that time. Placido’s genius in using a calibrated steel ball of known curvature as a baseline for his reflected concentric rings, cleverly photographed with the cameras of the day, allowed him to make accurate, but laborious, hand plotted maps of the ocular surface for direct comparison and evaluation.
Placido had some challenging obstacles and limitations to encounter. The first wearable contact lens would not be developed by pioneers Fick, Muller and Kalt2 for another 8 years and the utopian concept of instant computer analysis would not have been part of Placido’s wildest imagination as he tediously plotted his accurate observations.
Plaster of Paris, another effective Victorian method of measuring corneal shape is disturbingly and unacceptably brutal on the delicate tissues of the ocular surface. Although this technique was allegedly used by the developers of early contact lenses, their practice and research was exclusively reserved for cadaver eyes. Early designs of blown glass 19th-century scleral contact lenses show intimate knowledge not only of central corneal curves but to the limbus and beyond.
Keratometry
Enter the Keratometer. A simple, inexpensive, non-invasive, easily operated instrument which would give instant, reliable and repeatable results. Not yet had Queen Victoria relinquished her throne, and the theory of measuring smooth regular, spherical…even toroidal curves, consigned the theories of Placido to the forgotten cellars of science, for around a hundred years or so….
Working on optical principles documented by Christopher Scheiner3 (a pre great plague German mathematician and astronomer) the Ophthalmometer, or Keratometer as it was later known, was re-invented several times by Ramsden, Home, Von Helmholtz et al. The machine was able to provide optical professionals with the baseline information that they needed to instantly start fitting contact lenses. The famous, infamous, or some might argue notorious ‘K’ reading, became an instantly recognised and recorded evaluation of corneal shape for many generations of dedicated practitioners.
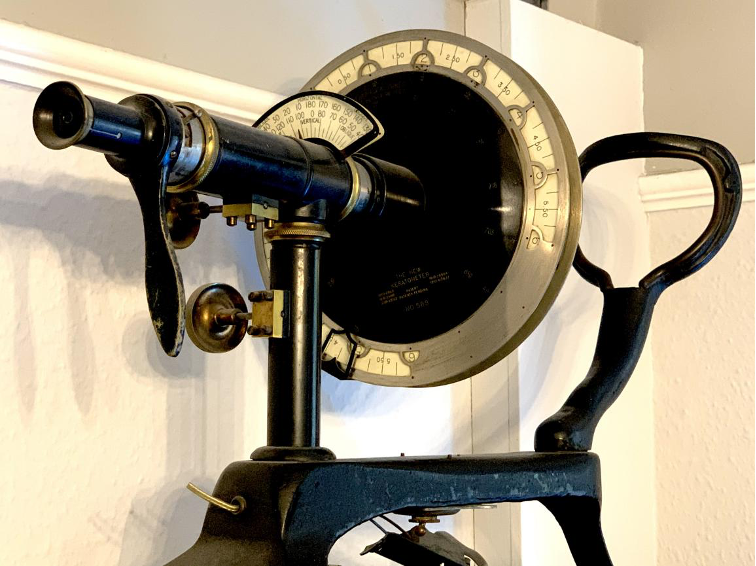
Fig 1 – ‘New’ two-position Keratometer circa 1920. Optical principle has not changed since the Victorian era. Image courtesy of Mr Brian Tompkins.
Students and mature post-graduates have used ‘K’ readings for decades. Some will have used the Keratometer in a more imaginative manner, successfully measuring Non-Invasive Tear Break Up Time (NITBUT). The more experienced professional eye is perhaps able to evaluate poor tear film quality, corneal irregularity, contact lens flexion – or even use the dated machine as a make-shift radiuscope4 in an emergency.
The Keratometer owns one major Achilles Heel and fundamental limitation – it is only able to cope with an arbitrary central 3 mm measurement. Considering that the average horizontal corneal diameter is 12mm, it is easy to calculate, using schoolboy mathematics, that the evaluation of a central corneal area 3mm in diameter will leave 93% of the corneal surface to the imagination of the observer.
Corneal shape
The central ‘corneal cap’ is often spherical, or sphero-cylindrical on a ‘normal’, or regular eye, but corneal eccentricity (rate of flattening) is impossible to consider or measure using the Keratometer. Indeed, the radius of curvature on a regular cornea (or if preferred dioptric value), can easily change by as much as 7.5mm or 35 dioptres from centre to periphery. On an eye with advanced Keratoconus, the corneal curve may change by over 60 dioptres across the visual axis, and an eye with ‘forme fruste’ Keratoconus, or Pellucid Marginal Degeneration, with corneal apex 2.5 mm below geometric centre may be misdiagnosed altogether by the Keratometer. A potentially debilitating corneal dystrophy or early signs of post-refractive ectasia will be a ‘no go’ area for the limitations of a Keratometer.
Topography
3mm, 5mm and 7mm zones
Placido would gawp in awe at the speed and accuracy of the modern day Videokeratoscope. A simple analysis of Placido rings (Scheimpflug based systems may be a preference), firmly fixed in the archives of physics history, give an instant, colour-coded map. Topography – defined as ‘’The arrangement of the natural and artificial features of an area’’, introduces professionals to the concept that every cornea is a unique and constantly changing landscape. A cornea is as unique as it’s host’s personality, as individual as any fingerprint.
Placido would be so proud of our instant ability to subdivide the region into three separate concentric zones, 3mm, 5mm and 7mm. Corneal cap at 3mm, so crucial to visual performance and comparison with refractive astigmatism. The 5mm zone where astigmatic errors typically reduce in magnitude, or extend onwards towards the limbus and beyond – and lastly 7mm and farther where a typical cornea flattens quickly to form a tangent angle, rather than a curve, so well documented by the scholars of Orthokeratology and mini-scleral contact lens specialists.
Placido would stand back in wonder at the sight of the oblate, post-refractive surgery cornea, maybe post keratoplasty cornea, with notably steeper mid-peripheral curves at 5mm and more and would marvel in the ability to use the difference mapping tool to accurately measure visual variability on blink, or monitor subtle signs of change in progressive corneal disease and subsequent referral for Collagen Cross Linking (CXL) procedures.
Keratoconus
For centuries Keratoconus has been considered to be a debilitating disease and the contact lenses developed by Victorian pioneer Adolf Fick in 1888 were specifically considered for this unfortunate cohort. Time established estimates of 1 in 2000 incidence have now been widely disregarded with the advent of corneal topography. Early stages of the disease are easy to spot5 and screening programmes would indicate 1 in approximately 4006 to be a more likely estimate of prevalence. Additional future study may indicate even higher recordings in specific geographical regions7 and an early diagnosis with careful, dedicated management may help to reduce, or possibly eliminate additional disease progression.
Dry Eye
Arguably an essential tool in the assessment and management of ‘dry eye’, the corneal topographer provides valuable, visual perception. NITBUT, in glorious technicolour, with sequence recording facilities available on some instruments. Patient engagement and understanding at its most complete.
Ever get fed up and wondered why that patient is dancing up and down with their responses when using a cross cyl? Evaluate with a corneal topographer and it is possible to check and demonstrate extremes of variability of cylinder axis and cylinder power between blink. Best recorded acuity below expectation? Check for corneal asymmetry or dystrophy – rarely is a perfectly symmetrical cornea found; it is a fingerprint, with peculiarities exaggerated and expanded by dry eye disease.
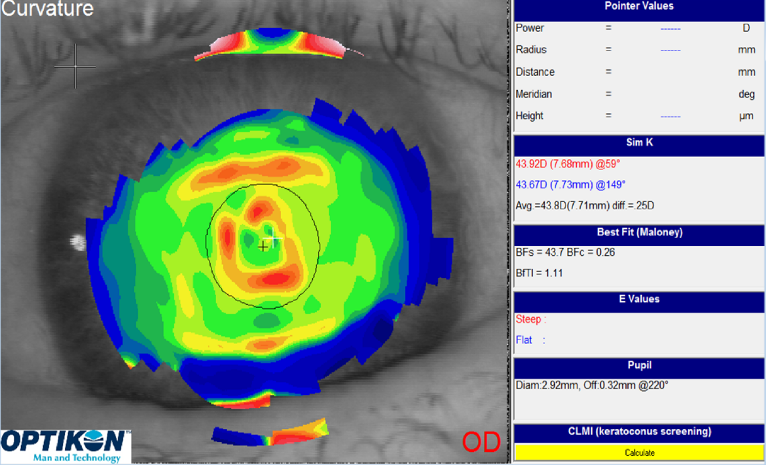
Fig 2A – Ocular surface dystrophy identified and recorded by corneal topography.
Fig 2B – Ocular surface after 1 month of intensive ‘dry eye’ management.
Contact Lens Fitting
Covid-19 has altered our lives in so many ways and one major benefit of the corneal topographer is virtual contact lens design – eliminating the need for the patient to be present in the room. The importance of the practised, polished techniques used when capturing imagery has been well documented over the years, but lens fitting from accurate imagery has never been more important than in our current, troubled times.
Corneal GP lenses8, Orthokeratology contact lenses and Mini Scleral contact lenses can all be designed from accurate corneal maps. The necessity of evaluating multiple lenses on eye has gone. There is absolutely no need for expensive, time consuming and uncomfortable work in close patient proximity. The vast majority of evaluation can be completed from a single quality corneal map and contact lens manufacturers are happy to design lenses on your behalf from quality imagery supplied digitally. The ability of a corneal topographer to evaluate toricity beyond the limbus, even the position and elevation of nuisance pingueculae may not be within the scope of all instruments, but some machines take us by surprise, and into the realms of optical witchcraft.
Many manufacturers and designers of specific contact lens profiles install their unique fitting concepts on modern instruments, giving eye care professionals the ability to change base curve, diameter, peripheral curves and other parameters at their leisure. Studies have considered the accuracy of contact lenses fitted on empirical information9 – the key to success would appear to be with the operator’s experience and skills.
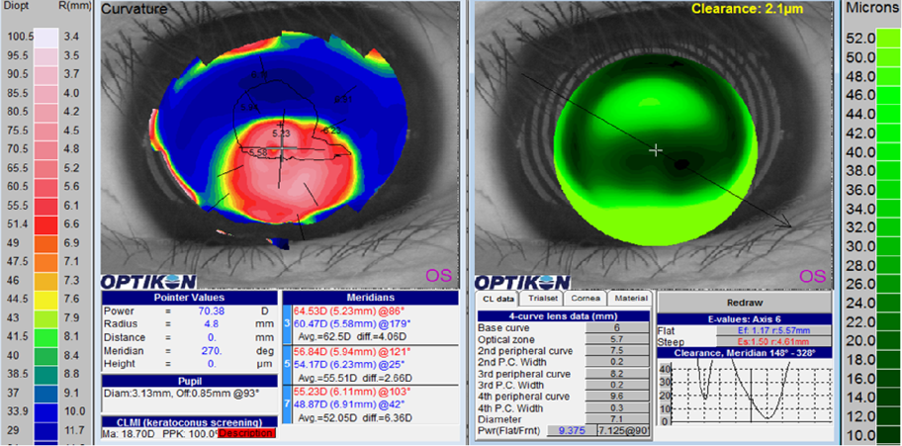
Fig 3 – Virtual fitting of RGP corneal contact lens on Keratoconic eye with inferior cone.
Dark Ages
2020 may not be remembered for the best of reasons. This year, with positive optical connotations, will no doubt go down in history as a dark and disturbing time aligned to the disasters and epidemics of the middle ages. Professor James Wolffsohn’s consideration and suggestion in 201710 indicated that the Keratometer should perhaps be consigned to a previous era; a relic, a museum piece of the darker ages. The corneal topographer allows optical professionals a colourful opportunity to see the light at the end of the tunnel and it may be time now to transport into greater awareness and understanding of true corneal shape. Placido’s genius appeased.
1. Cavas-Martinez F. et al Corneal topography in keratoconus: state of the art Eye Vis (Lond). 2016; 3: 5.
2. Rathi V M. et al Scleral lens for keratoconus: technology update, Clinical Ophthalmology 2015 Oct; 9: 2013-2018.
3. Martin R. Cornea and anterior eye assessment with placido-disc keratoscopy, slit scanning evaluation topography and scheimpflug imaging tomography, Indian Journal of Ophthalmology 2018 Mar; 66 (3): 360-366.
4. Kumbar T.et al Correlation of Back Optic Zone Radius measurement of rigid contact lenses with radiuscope and keratometer, Contact Lens Anterior Eye 2012 Dec; 35 (6): 282-4.
5. Fam HB, Lim KL. Corneal elevation indices in normal and keratoconic eyes. Journal of Cataract Refractive Surgery. 2006;32:1281–7.
6. Godefrooj DA. et al Age-specific incidence and prevalence of keratoconus: A nationwide registration study, American Journal of Ophthalmology 2017 Mar;175:169-172.
7. Netto EAT. et alPrevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia, British Journal of Ophthalmology 2018 Oct;102(10):1436-1441.
8. Van der Worp E. et alOptimising RGP lens fitting in normal eyes using 3D topographic data, Contact Lens Anterior Eye 2002 Jun;25(2):95-9.
9. Szczotka LBClinical evaluation of a topographically based contact lens fitting software, Optom Vis Sci 1997 Jan;74(1):14-9.
10. Wolffshon J S.Keratometry – A technique that should be relegated to the clinical dark ages? Contact Lens Anterior Eye 2017 Dec;40(6):357-359.
Thank you to Nick Howard for contributing to Global Insight.
Nick Howard qualified as a Contact Lens Optician in 1984, working primarily with challenging ocular conditions and complex contact lenses. Part-time lecturer, trainer and presenter at conferences, hospitals and Universities at local, national and international events. Winner of prestigious Contact Lens Optician of the Year award in 2012, Fellowship of the BCLA and currently a BCLA Council member and Faculty speaker. Now working in two Lancashire hospitals fitting speciality contact lenses, plus independent practice, developing innovative techniques for the management of myopia and dry eye.
