All Lenses Considered
The Decade of Soft Specialty Lenses: 2020-2030
by Eef van der Worp
This is such a fun and interesting field we are in – the specialty contact lens industry. I have been in this profession for a few decades now, and there has never been a dull moment. After I graduated in 1993 from optometry school in the Netherlands, corneal GP lenses were high on the agenda. Corneal topography had just entered the scene and promised – and proved – to be a very exciting development and groundbreaking in many ways. My PhD project was, in fact, on corneal GPs and how to prevent corneal desiccation and improve comfort – (indeed with the help of corneal topography).
Therefore, the decade from 1990-2000 will personally always resonate as ‘the decade of corneal topography’ and how it could aid corneal GP lens fitting. Then, in 2000, there was this huge roadshow on orthokeratology and that train to jump onto. The decade roughly from 2000 to 2010 seemed to mark the rise of orthokeratology, certainly from a peer-reviewed point of view – as well described by Mark Bullimore and Leah Johnson in Contact Lens & Anterior Eye recently.
The Demise of Corneal GPs
Around that time in 2010, ‘the demise of rigid gas permeable lenses‘ was declared by Nathan Efron. Interestingly though, not much has changed since then. Or actually, something has changed: the decline in rigid lens fits worldwide stopped pretty much at the moment Efron made his prophecy. According to the 2020 Eurolens research data on 13,311 lenses fit in 25 countries, there is hardly a visible decline in rigid lenses over the last decade. If anything, it is the opposite (a slight increase). This includes scleral lenses, which of course have been a bit of a game-changer for the industry.
Scleral Surge
Needless to say, the last decade for the specialty lens field has been the decade of ‘sclerals’. Rute Macedo-de-Araújo from Portugal did the annual ‘scleral lens publication count’, resulting in a huge surge in papers in 2020. The graph in figure one speaks for itself, and this exemplifies the real interest and surge in scleral lens fitting worldwide.
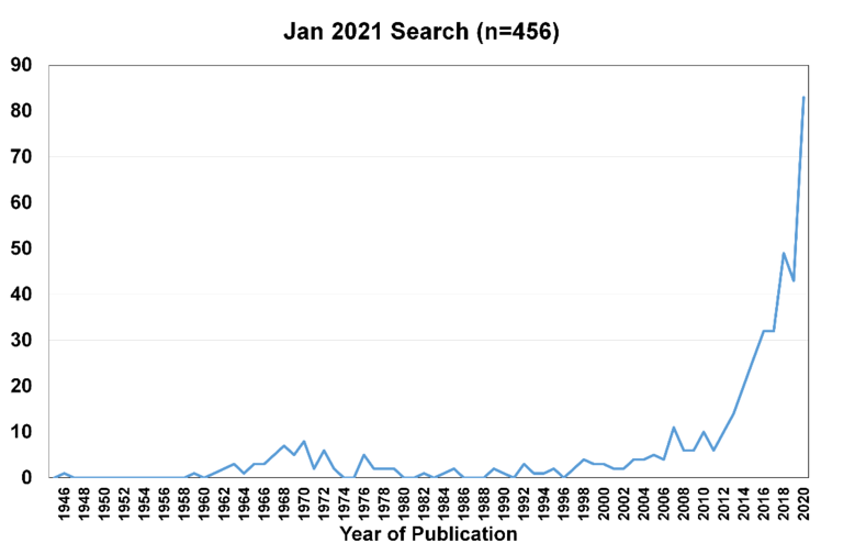
Figure 1: Scleral Lens Publication Count 2020
20/20 In Hindsight
The past year was definitely not what anyone had envisioned. Soon after many of us met at the Global Specialty Lens Symposium 2020 in Las Vegas, the world closed down, and we still haven’t recovered from that. But 2020 may prove to be a pivotal year in many ways. After corneal GPs and corneal topography, orthokeratology and sclerals – what is next? In my (20/20+) view, it has to be soft specialty lenses.
The Decade of Soft Specialty Lenses
This may resonate best by looking at the Global Education Series – the worldwide generic specialty lens lecture series that has been an ongoing success, made possible by the exclusive and continuous support of Contamac.
The 2020 series looked a bit different, with obviously a decline in live lectures. At the same time, more online events took place and other online content was developed – with activities in various countries including but not limited to India, South Africa, Canada, USA, Colombia, and of course Europe. Myopia management (including orthokeratology – still one of the intervention methods with the best track record on file) was a popular topic in the 2020 Global Education Series (and rightfully so). Plus scleral topics continue to be popular. But nothing beat the popularity of interest in specialty soft lens fitting in the past year. Including – of course – Class 2020, with the topic even presented as the opening lecture of this spectacular event.
2020 also marked the 40th edition of SoftSpecialEdition newsletter, kindly supported by Contamac as well as part of the Global Education Series. Numerous experts (40 to be exact) have shone their light on soft specialty lenses and their future in the column that kicks off each newsletter. The fall edition of the newsletter also marked the first column by me as editor and as an exception to the rule. As I wrote in that anniversary column, I envision that the next decade could be the decade of soft specialty lenses. To name a few considerations: we live in a day and age in which everything is customized. The technology to do so is available, and customers demand it. Artificial intelligence is going to help us tremendously in terms of distinguishing the normal from the challenging eye to decide when to ‘go custom’ and when standard lenses would satisfy.
Higher-order Aberrations
Higher-order aberrations are going to play a much bigger role, and correcting these can only be implemented if we are customizing lenses. Instrumentation to measure the true optical status of the eye is increasingly available and affordable.
The two most promising modalities in our industry for soft lens customization are, without question, multifocal lenses and myopia control. But because the eye is such a unique piece of work, it needs a custom made lens to provide different optics at different times to be successful. Or – as Scott Read described it in a more recent column of the newsletter: ‘while it is clear that significant work is needed in multiple areas to better understand the optical effects of multifocal lenses and how they can optimally impact childhood eye growth to achieve improved myopia control outcomes, results to date suggest that clinically significant effects can be achieved with current lens designs, with the promise of improved outcomes in the future as our understanding of the optical effects on eye growth continues to improve.’
Dropouts
One of the main challenges within the soft lens category traditionally has been, and remains, the large dropout rate. Calculations by Phil Morgan show that small reductions in dropout rates can cause significant changes in the overall lens wearer base. Simple calculations show that if we could reduce the dropout rate by as little as 3.5% between 2020 to 2040, we could double the number of contact lens wearers in our practices.
The previous fact prompted a few experts in the field including James Wolffsohn from Aston University in the UK, Lyndon Jones from Waterloo University in Canada and myself to look at the topic of soft lens dropout, with a particular emphasis on lens fit and lens fit options, including replacement frequency and material choice. Our intention was to aim for a reduction in dropout rate in the order of magnitude mentioned above. A number of sessions at various conferences focused on the topic, and a few publications resulted from that including ‘Dropping the Dropout Rate’ in the May issue of Contact Lens Spectrum and an editorial in Contact Lens & Anterior Eye: ‘When was the last time you FITTED a soft lens’.
Figure 2: Dropping the Dropout Rate in Contact Lens Spectrum
What is Normal?
For a good strategy, it seems that first and foremost we need to find ‘normal eyes’ – or NEMOs (normal eyes measured ocular surfaces). Because if we have normal eyes, this is most likely where our normal, standard lenses will come in and in fact is what they were designed for.
This is where technology comes to the rescue. Based on corneal diameter, eccentricity of the cornea if available (the amount of flattening toward the periphery) and the central keratometry values (in that order of importance), we can get a rough idea about the overall shape of the eye by calculating the overall sagittal height of the ocular surface. Corneal topographers are typically pretty good at measuring the cornea – and extending this out to 15mm (our workbench) based on extrapolation. Newer instruments can also directly measure this. As described in a web-based series EEF-online: it is not about flattening the curve, it is about altering the sagittal height to make a difference.
In a recent Pacific study, 44 daily disposable lenses, reusable lenses and toric lenses were analysed and put into graphs and grids for comparison. From the bulk of data this generated, a couple of things can be derived. First, it becomes obvious that lenses with a given base curve (BC) on the package are not interchangeable. In other words, one ‘9.0’ BC lens is not the same as the next ‘9.0’ BC lens. For daily disposables, the difference (n=3) was as much as 384 microns between these lenses; in the reusable lens category, a 430-micron difference was found between two 8.4 BCs.
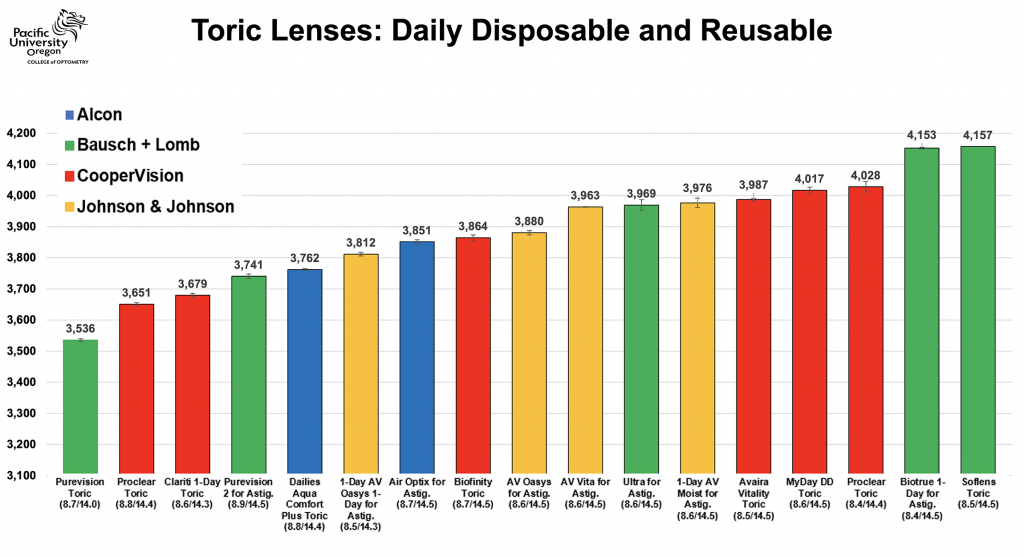
Figure 3: Pacific Study – Daily Disposable and Reusable Toric Lenses
What the data also made clear is that if a certain lens brand has two BCs, then the difference between them was typically somewhat limited. The average difference in sagittal height between two BCs of the same design was 274 microns. As a reference, the total range of normal eyes from flattest to steepest is at about 900 microns. Hence, there is an obvious need for customized lenses on either side of the spectrum.
Think Inside-the-box (and outside)
This means we need to think ‘inside-the-box’ quite literally sometimes. We have to start finding NEMOs, then we can start with fitting standard ‘off-the shelf’ lenses. Maybe a box of 30 lenses of a given manufacturer is the best option for that individual. It seems unwise to replace the superb and sophisticated lenses that we have in the frequent replacement category – cast-moulded and ultra-thin – with relatively thick lathe-cut custom-made lens designs that typically are also more expensive too.
However, the other way around is true too: it does not make sense to fit a standard lens to an out-of-standard eye – it’s a losing game. If we have a more extreme, but non-pathological eye shape – e.g., at either the left or right end of the bell curve – then we may consider looking at other lens alternatives. This is where extended-parameter lenses or tailor-made lenses come in.
Soft Lens Puzzle
While this could be a good first step up in fitting soft lenses and actually getting some ‘grip’ on the soft lens fitting again, the method of just putting a lens on the eye ‘and hoping for the best’ is hardly scientific.
In a way, fitting scleral lenses has more science and skill to it than with our most popular lens out there: the soft lens. Currently, soft lens fitting actually copies what we do with sclerals: we typically take the ‘middle lens’ from the trial set and see if it works. If there is too much clearance, we reduce the sagittal depth or vice versa. With the current Pacific soft lens graphs, we can do the same. This soft lens equivalent of ‘clearance’, ‘vault’ or tear reservoir thickness is what we call the fitting factor. A standard soft lens has to be some degree steeper (higher sag value) than the ocular surface in order to fit right.
Current research is looking into that: defining the exact right amount of difference between the lens and the ocular surface, where material properties, temperature (on-eye versus room temperature) and a few other considerations play a role. Stay tuned in 2021 for more on this.
All Lenses Considered
In my view, soft lenses have just scratched the surface when it comes to their potential and have the best prognosis for innovation and growth. There is no question in my mind that if we customize soft lenses to the individual ocular surface (if needed) and to the optical aberrations of the individual (at a given age), we’ll be able to get much further.
This will be beneficial for all of us if we can first somewhat reduce the dropout rate and gain more effectiveness in terms of multifocal and myopia management lenses. The future will tell us. But that future is, at least partly, in our hands. I’ll check back with you in 2030 to see where we are. Wishing you a happy new decade.
Thank you to Eef van der Worp for contributing to Global Insight.

Eef van der Worp is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as head of the contact lens department at the school for over eight years. Eef received his PhD from the University of Maastricht (NL) in 2008. He now runs his own research & education consultancy ‘Eye-Contact-Lens’ which is based in Amsterdam (NL), and gives courses on ‘How to Present’. He is a fellow of the AAO, BCLA and the SLS, a lifetime fellow of IACLE and an honorary life member of the Dutch contact lens association ANVC.
More by Eef van der Worp:
