Scleral Lens Non-Wetting: Is it the lens or the lid?
Scleral lenses have become an increasingly popular way of correcting vision for the irregular cornea patient as well as the individual with ocular surface disease. As more scleral lenses are prescribed and worn, problems both big and small can start to become frequent enough in numbers to create discussion among lens fitters. One of those problems is the matter of lens surface non-wetting. This is an increasingly common post found on a social media site for scleral lens fitters:
“Ok all of you helpful scleral lens fitters. Anterior fogging. Please don’t even say the usual, you know, the peroxide, the Progent, and on and on.
Here is my issue. I bet I am not the only one. When a lens fogs on the anterior surface within minutes. What on earth do you do?
I have patients who we have tried lenses from at least three companies. No matter what you read, no matter what you do, the stupid thing fogs. And yes, I have inspected meibomian glands. And yes I have treated for dry eye…and yes and yes and yes. I take a brand new lens out of a wet vial, I fill it with unpreserved saline…I put in the drop of artificial tears. The front surface becomes opaque. I wish it were just one patient or one lab. How on earth can these treat dry eye if a relatively asymptomatic patient completely fogs the front? How on earth?“
Do you sense the frustration? This is something that we blame on external lid health, lens deposits, lens surface condition, solutions, and so on. But perhaps we are not looking in the right place for the culprit?
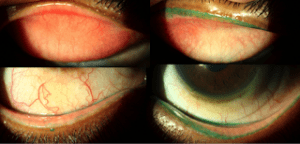
I recently examined a corneal GP wearer with similar symptoms that had bounced from one provider to the next looking for an answer to her lens fogging issue. After a lengthy discussion and observation of her lens and ocular health, I stained her with lissamine green and everted her lids. The degree of lid wiper epitheliopathy was unexpected.
Notice how the area of staining follows exactly the area of contact with her GP lens? She clearly has severe lid wiper epitheliopathy, and no wonder her lens will not wet properly, her “windshield wiper” is completely useless in distributing the tears across her lens surface. After this, I started observing all of my scleral lens wearers, to find this same issue was all too common.
This is a gentleman that wears a scleral lens in one eye and no correction in the other. Notice the remarkable difference between the lids of the right eye versus the left eye. While this patient was only mildly symptomatic, it has become typical of many of the scleral lens wearers I have seen lately.
Why does this occur? I believe friction is the major cause, with the lens pushing the lid out with each blink, as well as providing a plastic surface for the entire span of the blink, the amount of friction that the upper lid encounters with a scleral lens is far greater than encountered with a standard corneal GP or even a soft lens which lies flat against the eye. In addition, many practitioners are moving toward Hydrogen Peroxide care systems, which provide little in the way of lubrication or conditioning to the anterior lens surface.
How do we combat this? In the short term, I have been educating patients about their lids and the friction that occurs and recommending frequent lubrication while wearing lenses, not for symptoms of dryness, but for reduction of lid wiper epitheliopathy and eventually, better anterior lens surface condition. Debriding of the lid wiper is another method for improving the condition of the lid, though this must also be followed up with frequent lubrication after debriding.
Ultimately, the best way to manage this is to have a more wettable lens surface, one that significantly reduces friction continuously. A new surface treatment that is currently being tested for FDA approval on GP lenses, Hydra-PEG, brings hope for managing this situation. This treatment is a covalently bonded layer of Polyethylene Glycol, a common and effective ocular lubricant that affixes to the lens surface in a permanent fashion. Having a layer of lubricant on the lens surface improves surface wettability, decreases visual fluctuations, and improves comfort.
An example of this is demonstrated in the following case. A 68 year old male was using scleral lenses for extreme dry eye post chemotherapy. While generally happy, he noticed issues with vision fogging throughout the day. Upon examination, a very short tear break up time (TBUT) was noted over the lens surface (Picture 1 and 2). After remaking his lenses with Hydra-PEG he reported improved symptoms and examination revealed a significantly prolonged TBUT on the anterior lens surface (Picture 3 and 4).
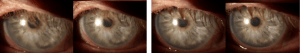
(Picture 1) image of the light reflex immediately post blink and (Picture 2) image after 10 seconds – note dispersion of the light reflex; (Picture 3) image of the light reflex immediately post blink and (Picture 4) image after 10 seconds – note the light reflex staying sharp
Anterior surface non-wetting issues with scleral lenses is a common problem that is a challenge for practitioners to remedy. I am hopeful that the introduction of Hydra-PEG in the near future will provide a breakthrough in how we prescribe scleral lenses to all patients, not just those that are symptomatic.